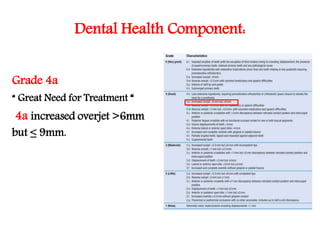
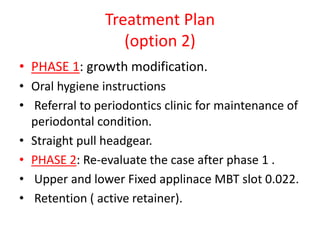
This case presentation summarizes the orthodontic treatment of a 12-year-old male patient. He presented with a class II malocclusion due to a skeletal class II jaw relationship. Treatment options included functional appliance therapy using a MOA or headgear. The treatment plan was to first use a functional appliance to modify growth, followed by fixed appliance therapy using MBT brackets to align the teeth and achieve a class I occlusion. Retention would involve a Hawley retainer with anterior bite plane. The functional appliance aimed to restrain maxillary growth and allow mandibular autorotation to correct the overjet and overbite.