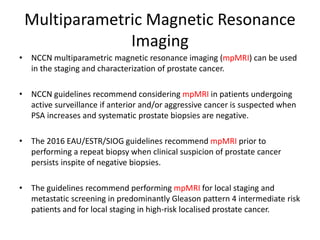
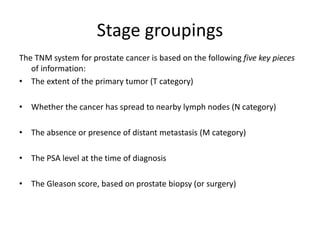
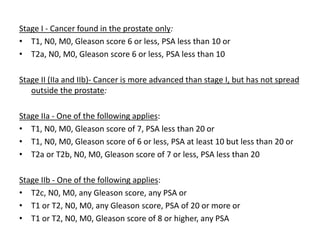
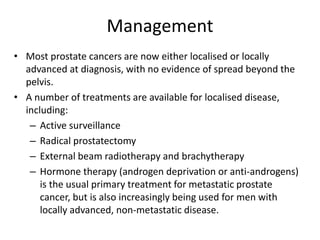
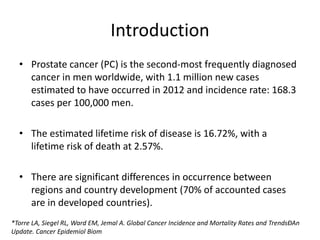
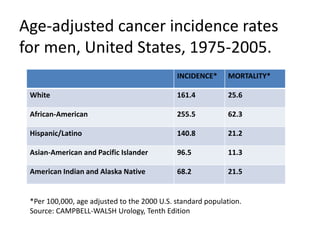
This document discusses recent advances in prostate cancer, including updated screening guidelines, diagnostic tools, biomarkers, staging, and treatments. It provides an overview of prostate cancer epidemiology and risk factors. Screening involves PSA testing and digital rectal exams for men aged 55-69. Multiparametric MRI and MRI-ultrasound fusion biopsies have improved detection of aggressive cancers. Staging involves bone scans, PET scans, and the TNM system. Biomarkers like PSMA and PCA3 are also discussed.
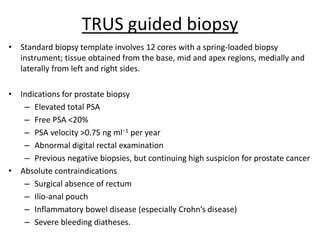
![Risk Factors
• Both genetics and environment play a role in the origin and evolution of
this disease.
(A) Familial and Genetic Influences
- Relative risk increases according to the number of affected family
members, their degree of relatedness, and the age at which they were
affected.
- Linkage studies have identified a number of prostate cancer susceptibility
genes, including RNaseL (hereditary prostate cancer-1 [HPC1] region,
1q23-25), ELAC2 (HPC2 region, 17p) and MSR1 (8p22-23).
- However, sporadic cancers account for about 85% of all prostate cancers
and about 15% are familial and/or hereditary.](https://image.slidesharecdn.com/caprostatefiinalupload-180815083345/85/Carcinoma-Prostate-Recent-Advances-7-320.jpg)
![Glutathione-S-Transferase Pi (GSTP1)
• GSTP1 belongs to a family of detoxifying enzymes that are
involved in metabolic reduction of electrophilic carcinogens.
• These enzymes are thought to be involved in the development of
prostate cancer.
• Elevated levels of GSTP1 CpG hypermethylation have been
detected in tissues from precancerous lesions (atypia and
prostatic intraepithelial neoplasia [PIN]) and within ejaculates,
urine, and plasma from men with prostate cancer. (Nakayama et al, 2003)](https://image.slidesharecdn.com/caprostatefiinalupload-180815083345/85/Carcinoma-Prostate-Recent-Advances-20-320.jpg)