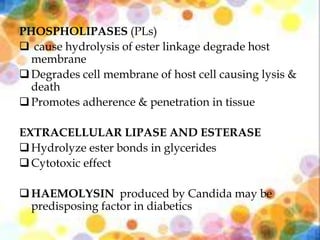
This document discusses oral candidiasis, caused by an overgrowth of Candida species in the oral cavity. It begins with an introduction to candidiasis and the most common Candida pathogens. It then covers the classification of oral candidiasis, including acute and chronic forms. Predisposing factors are discussed. The document delves into the clinical features and management of various types of oral candidiasis such as pseudomembranous candidiasis and denture stomatitis. Laboratory tests for diagnosis are also summarized, followed by an overview of antifungal drugs used to treat oral candidiasis.