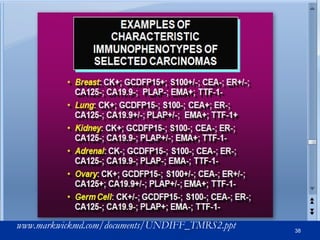
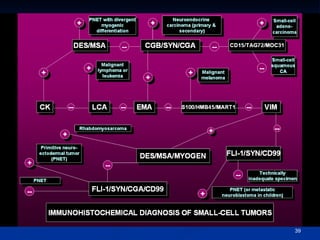
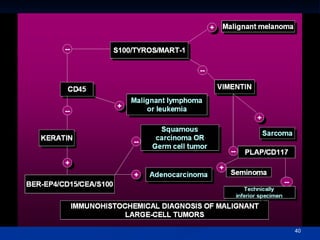
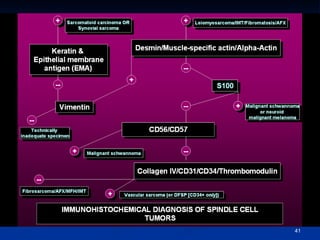
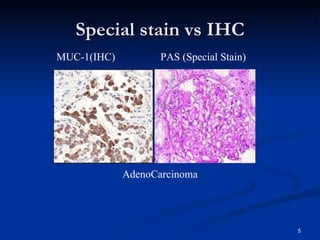
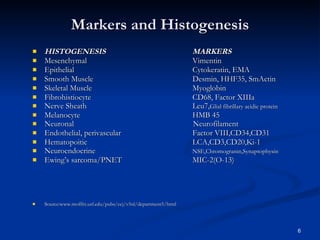
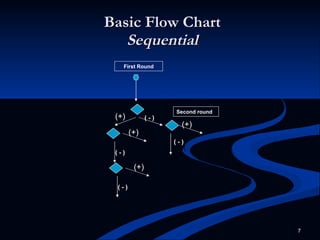
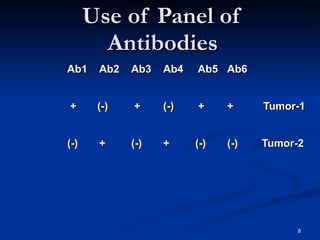
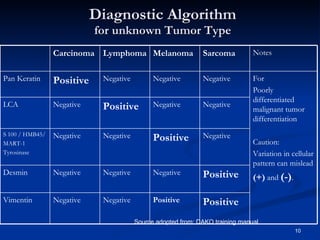
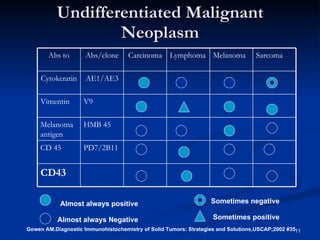
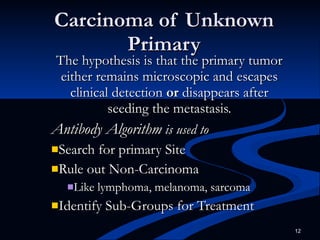
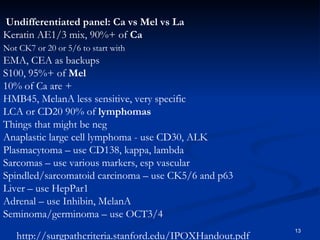
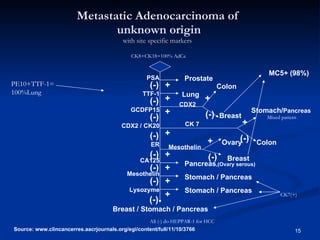
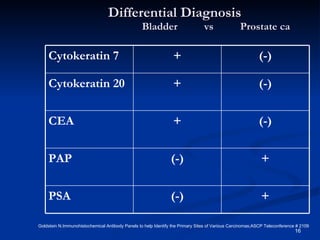
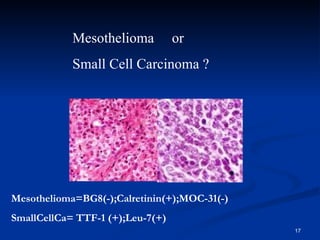
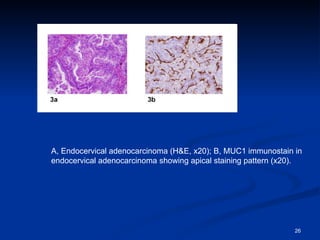
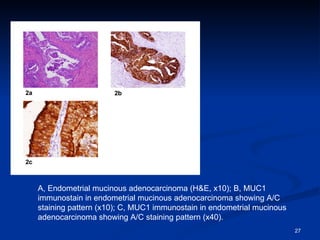
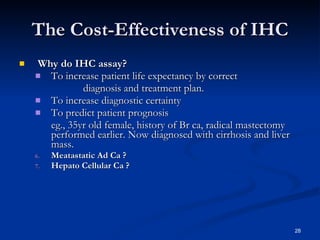
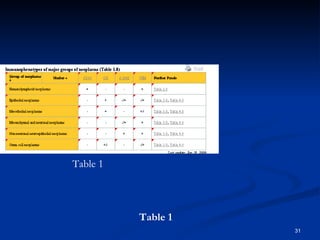
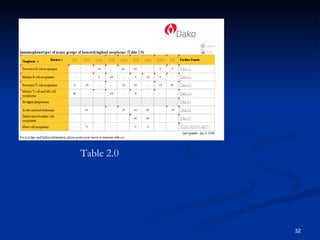
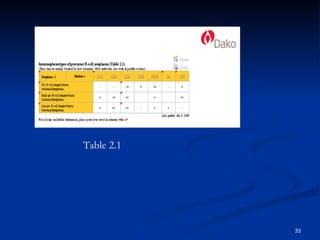
The document discusses the use of diagnostic algorithms and immunohistochemistry (IHC) in cancer diagnosis, emphasizing their role in determining tumor sub-classification and contributing to treatment decisions. It highlights the necessity of following specific algorithms based on morphological analysis and clinical history while noting that these procedures are not a substitute for professional pathologist judgment. Additionally, the document covers various antibodies used for identifying carcinomas and their implications on prognosis and treatment decisions.

![Threshold for Positivity * Positive Generally : unequivocal staining of =10% of tumor cells +/- + -/+ (-) Source: Dako antibody algorithm : >90% of tumors positive* : 50-90% of tumors positive* : 10-50% of tumors positive* : <10% of tumors positive* ? : Insufficient evidence [ ] : Staining of secondary (non-neoplastic) cell type ( ) : Staining dependant on antibody](https://image.slidesharecdn.com/cancerdxalgorithm-100327141448-phpapp02/85/Cancer-Dx-Algorithm-14-320.jpg)
![Thanks to DAKO & MMJ Biosystems Philippines, Inc . Address: Unit 206 CYA Land Bldg. (formerly LTC Corporate Center Bldg.) #282 EDSA Extension Cor. P. Celle Street, Pasay City, Manila Tel. nos.: (632) 851-0192 to 93/489-1008 Telefax: (632) 853-3665 email: [email_address]](https://image.slidesharecdn.com/cancerdxalgorithm-100327141448-phpapp02/85/Cancer-Dx-Algorithm-36-320.jpg)