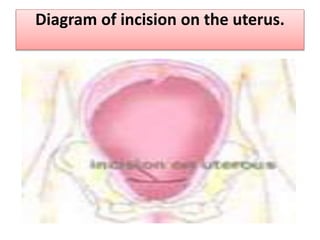
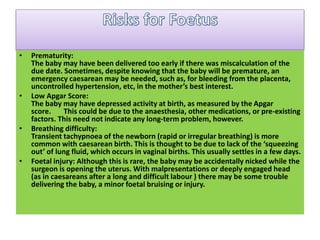
The document provides information about caesarean section (C-section), including that it is a surgical procedure to deliver a baby through incisions in the mother's abdomen and uterus. It notes that C-sections can be emergency or planned procedures. The preparation, procedure, and potential reasons for C-section are described at a high level.