The document discusses the utility of real-world evidence (RWE) in supporting value-based decision making from a provider's perspective. It provides three cases as examples:
1) Collaborating with a clinical community of practice to leverage RWE and optimize the impact of evidence-based innovations. Initial RWE proved the innovation would reach break-even in 22 months.
2) Creating a value case for the "triple aim" approach using RWE to better serve those with complex, high needs. Early evidence shows a regression to the mean in utilization.
3) Capturing value from research by defining the role of public services in commercialization and intellectual property. This includes using RWE to project health


![9
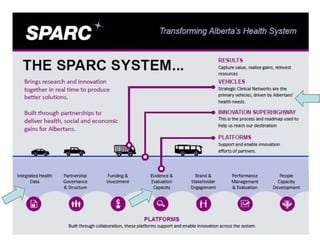
Case A: Collaborating with a clinical (provincial) community of
practice; a means to leverage RWE and optimize impact
• Strategic Clinical Network driven,
adopting evidence from abroad.
• Clear “measure of better”
• Literature guided initial projections.
• First two pilots yielded local RWE to
allow for a re-forecasting of cost -
benefit; process evolving.
• RWE proved conditional (notional)
break even/ payback in 22 months.
• Speed of innovation diffusion can be
at odds with research agendas.
• Risk free gains, verses practical value
creation. [Re-investment algorithm]
Source: published and approved ‘14-15
Operational Plan AHS Major Initiatives](https://image.slidesharecdn.com/cadth2015e62fenwick-150414090534-conversion-gate01/85/Cadth-2015-e6-2-fenwick-9-320.jpg)