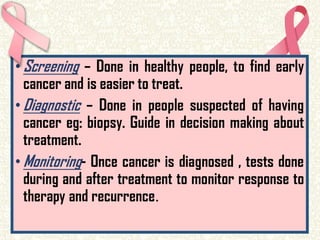
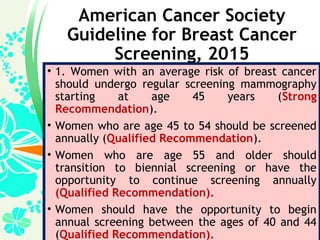
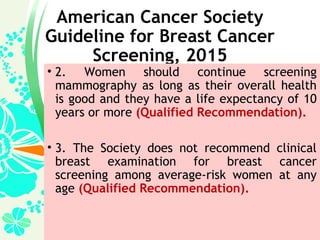
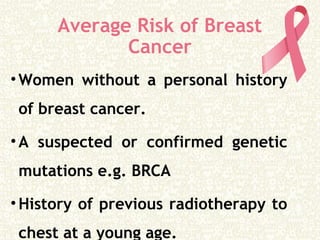
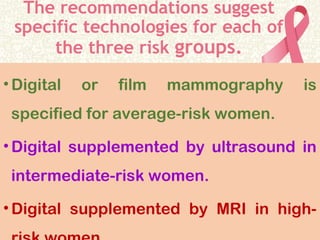
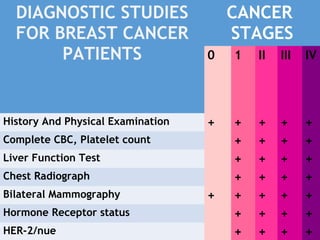
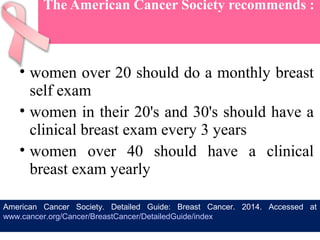
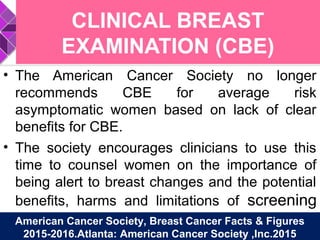
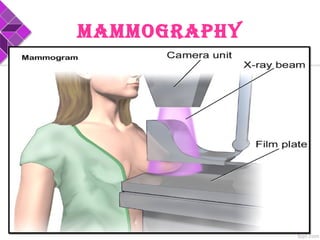
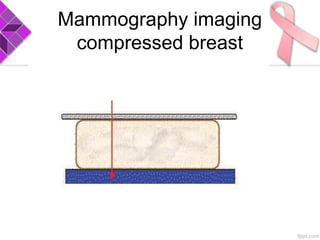
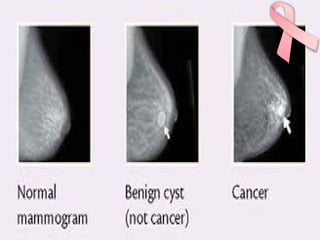
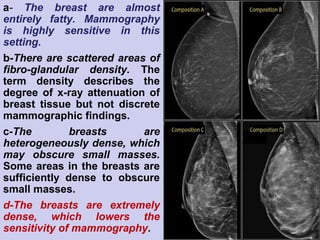
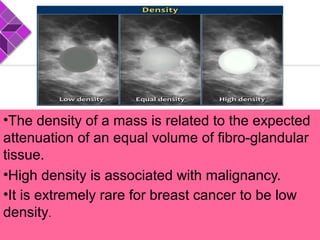
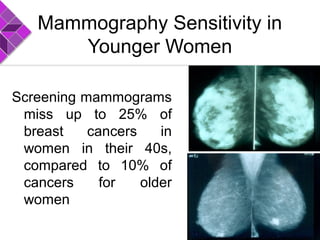
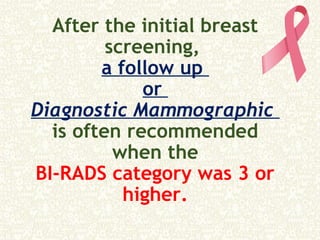
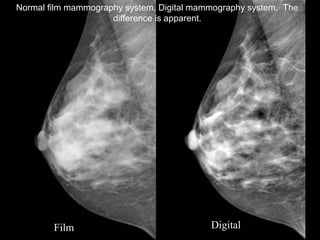
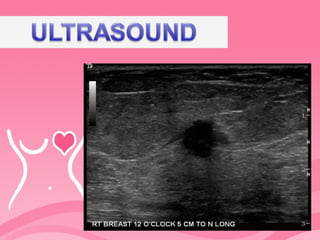
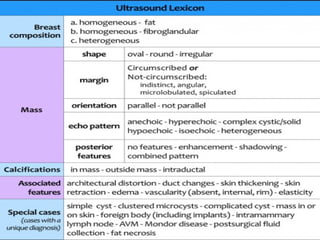
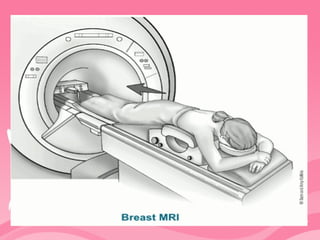
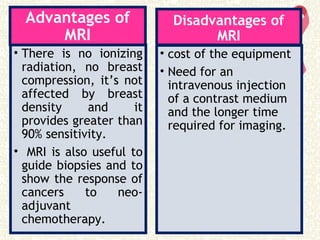
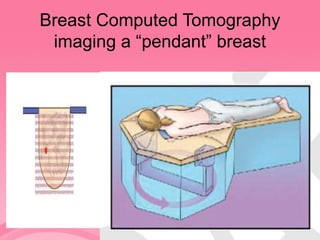
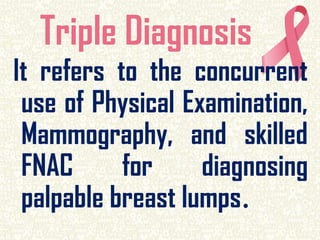
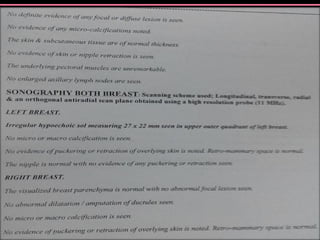
This document provides information on diagnostic tests for breast cancer. It discusses mammography, ultrasound, MRI, and clinical breast exams. Mammography is recommended for average risk women starting at age 45, annually or biennially depending on age. Ultrasound and MRI can supplement mammography for intermediate and high risk women. Clinical breast exams are no longer routinely recommended by the American Cancer Society. Early detection through screening improves breast cancer outcomes.