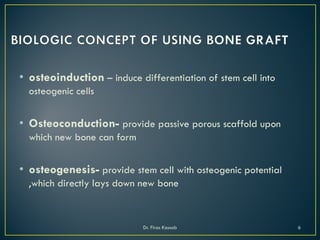
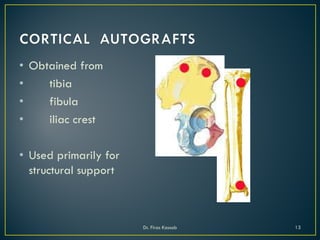
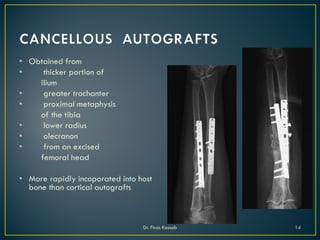
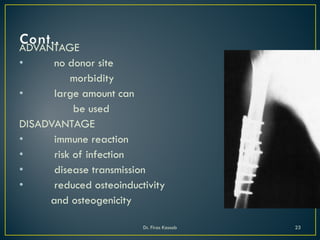
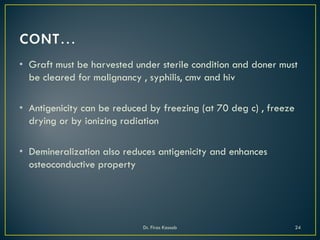
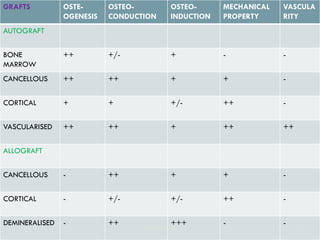
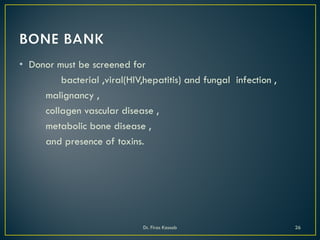
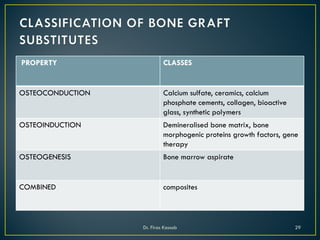
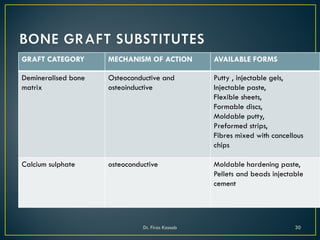
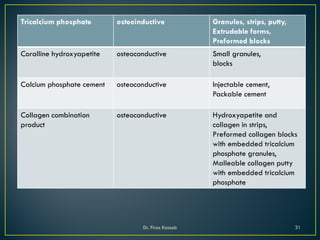
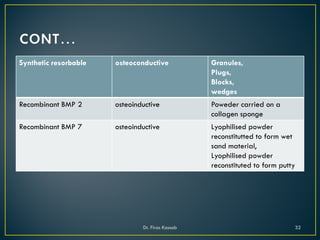
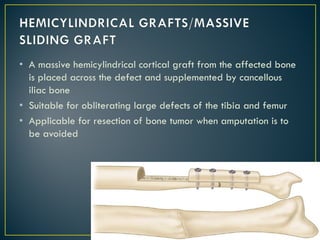
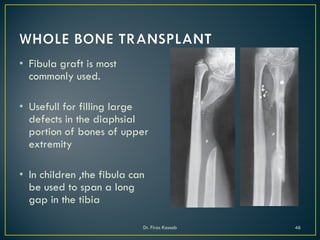
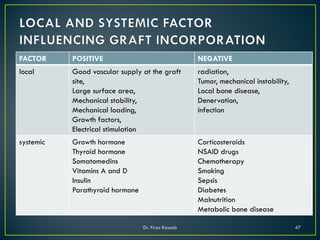
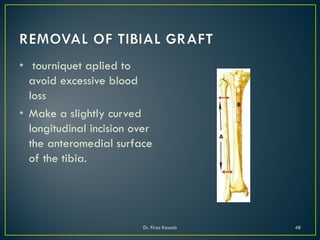
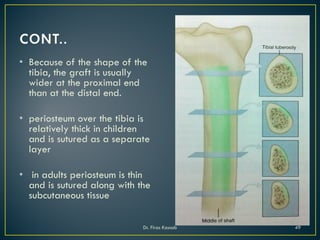
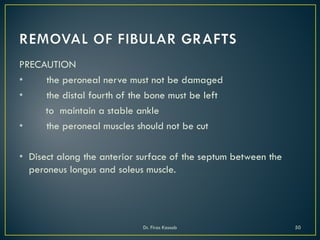
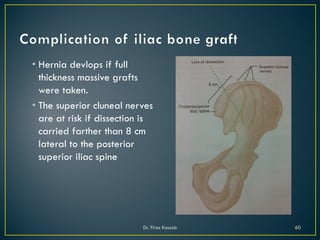
This document provides an overview of bone grafting presented by Dr. Firas Kassab. It defines grafting and bone grafts, discusses the history and objectives of bone grafting, and describes the biological concepts and techniques involved. Specifically, it covers the principles of osteoinduction, osteoconduction, and osteogenesis provided by different graft types including autografts, allografts, bone substitutes, and bone marrow aspirate concentrates. Common grafting procedures like onlay grafts and factors affecting graft incorporation are also summarized.