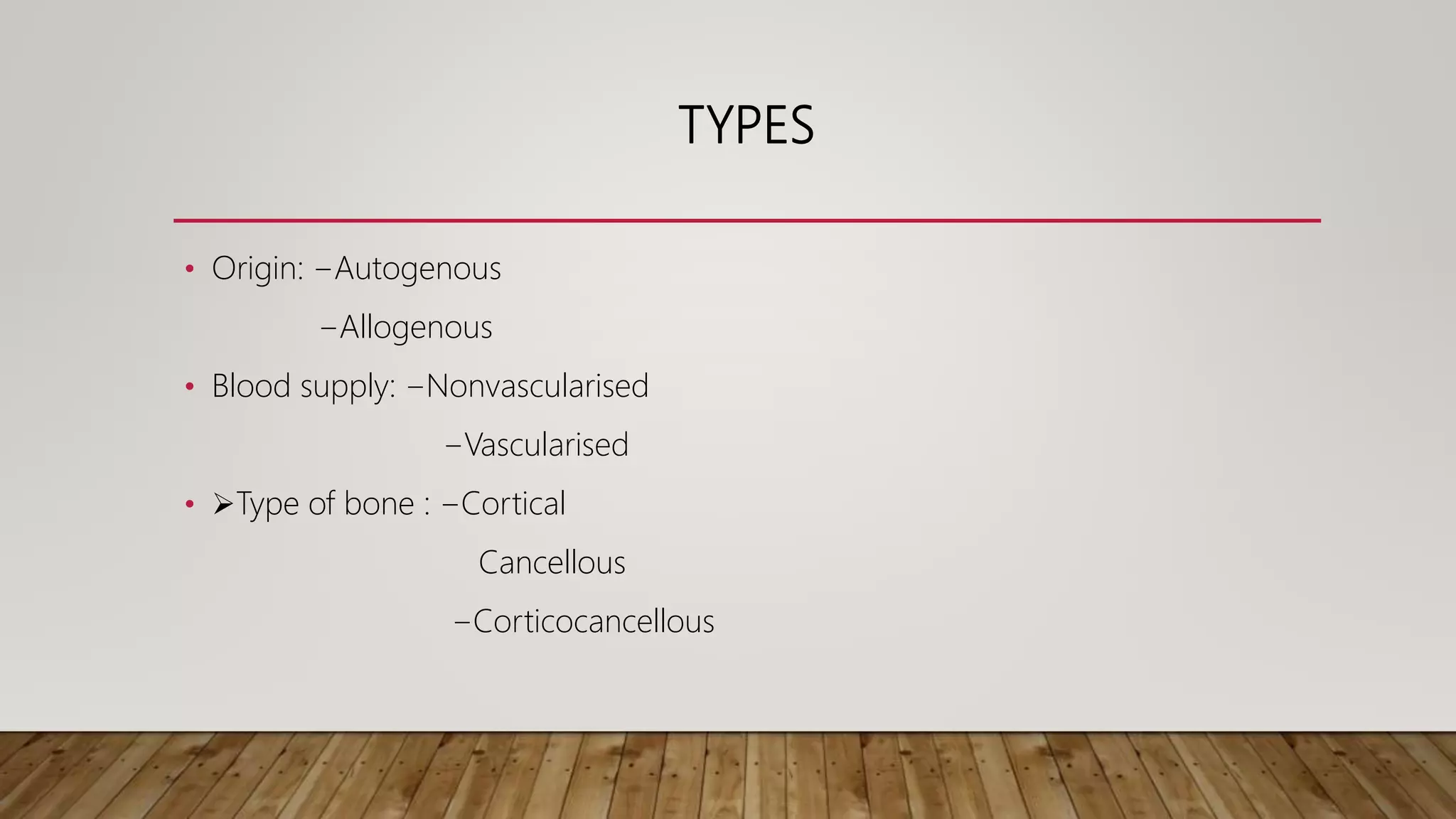
This document discusses bone grafting and bone graft substitutes. It begins by defining a bone graft as viable bone tissue implanted from a donor site to a recipient site to repair, restore, and regenerate tissue. It then covers the history of bone grafting, types of grafts including autogenous, allogenic, and xenografts. Specific bone graft techniques and various bone graft substitutes are also summarized, including calcium sulfate, hydroxyapatite, tricalcium phosphate, demineralized bone matrix, and bone morphogenetic proteins.