This document provides a comprehensive list of medicinal plants and their constituents organized by their pharmacological actions. It includes over 15 categories of actions such as analgesics, anti-parasitics, and ACE inhibitors. For each action, the plants and constituents are categorized from most potent to mild based on available research. The document aims to be a reference for practitioners on the actions of various herbs.




![Actions of Medicinal Plants 5 © 2007 Eric Yarnell, ND
H. Magnolia liliflora
I. Rubus spp, gallic acid
J. Salvia miltiorrhiza (Chinese sage) (Kang, et al. 2003)
K. Typha spp (cattail)
L. Zingiber officinale, [6]-gingerol
XIII.Androgenic
A. chyrsin (Matricaria recutita, Passiflora incarnata)
B. Tribulus terrestris
XIV. Angiotensin-converting enzyme inhibitor, ACE inhibitor
A. All mild.
B. see also diuretic below
C. Allium sativum (garlic)
D. lithospermic acid (Salvia miltiorrhiza)
E. proanthocyanidins (Crataegus laevigata, Vitis vinifera, Cupressus
sempervirens) (Meunier, et al. 1987)
F. secoiridoid glycosides eg oleuropein, ligstroside, excelcioside,
oleoside 11-methyl ester, oleoside (Olea europaea and Olea lancea
folium)
G. triterpenoids (Ganoderma lucidum) (Morigawa, et al. 1986)
Anodyne: see analgesic
XV. Anthelmintic, anti-amebic, anti-parasitic, anti-protozoal
A. By plant or constituent
1. Potent
a) ascaridol
b) aspidine
c) Azadiractha indica (neem)
d) Cinchona spp (Peruvian bark)—quinine, quinidine,
cinchonine, cinchonidine
e) Dryopteris filix-mas (male fern) radix (filicin)
f) emetine (Cephaelis ipecacuanha)
g) Staphysagria
h) Tanacetum vulgaris (tansy)
2. Mild-to-moderate
a) Allium sativum (garlic) bulbus (allicin)
b) Areca catechu
c) Artemisia annua (sweet Annie) herba (artemisinin =
qinghaosu)
d) Artemisia maritima herba (santonin)
e) berberine-containing herbs
f) Cucurbita pepo (pumpkin) seed
g) Cucurbita moschata seed
h) lapachol (Tabebuia avellanadae)
i) Melia spp](https://image.slidesharecdn.com/boeyarnell-herbactions-110417235042-phpapp02/85/Bo-eyarnell-herbactions-5-320.jpg)













































![Actions of Medicinal Plants 51 © 2007 Eric Yarnell, ND
I. polysaccharides (Echinacea angustifolia, E. purpurea)
J. polysaccharides (Aloe vera)
1. including stimulation of fibroblast activity
K. Symphytum officinale (comfrey) radix or herba (allantoin)
CLVIII. Xanthine oxidase inhibitor
A. morin (Chlorophora tinctoria)
1. moderately effective
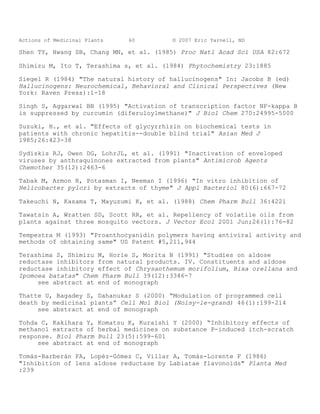
CLIX.References
Abbasoglu U, Sener B, Gunay Y, Temizer H (1991) "Antimicrobial activity of
some isoquinoline alkaloids" Arch Pharm 324:379-80
Adlercretuz H, Bannwart C, Wahala K, et al. (1993) "Inhibition of human
aromatase by mammalian lignins and isoflavonoid phytoestrogens" J Steroid
Biochem Mol Biol 44:147-53
Aghajanian G (1994) "Serotonin and the action of LSD in the brain"
Psychiatric Annals 2463(?? 26 #63?):137-41
Alonso-Osorio MJ (2001) “Phytotherapy and immunomodulators” Circular
Farmaceutica 59:40-44
Alsat E (1987) "Lomatium dissectum" Comp Med May/June:32-4
Ambros M, Lurton E, Boustie J and Girre L (1994) "Comparison of the anti-
herpes simplex virus activities of propolis and 3-methyl-but-2-enyl
caffeate" J Nat Prod 57(5):644-7
Anderson D, et al. (1991) "In vitro virucidal activity of selected
anthraquinones and anthraquinone derivatives" Antiviral Res 16:185-96
Anderton JG, Mantle D, Thomas TH (1996) "Antioxidant herbal preparations" J
R Soc Med 89(9):540 [letter]
Atta AH, El-Sooud KA (2004) “The antinociceptive effect of some Egyptian
medicinal plant extracts” J Ethnopharmacol 95(2-3):235-8.
see abstract at end of monograph
Barnard D, et al. (1992) "Evaluation of the antiviral activity of
anthraquinones, anthrones and anthraquinone derivatives against human
cytomegalovirus" Antiviral Res 1992;17:63-77
Beládi I, Pusztan R, et al. (1977) "Activity of some flavonoids against
viruses" Ann NY Acad Sci 284:358-64
Belidi I, et al. (1981) "In vitro and in vivo antiviral effects of](https://image.slidesharecdn.com/boeyarnell-herbactions-110417235042-phpapp02/85/Bo-eyarnell-herbactions-51-320.jpg)
![Actions of Medicinal Plants 52 © 2007 Eric Yarnell, ND
flavonoids" In Farkas, et al. (eds) Flavonoids and Bioflavonoids: Proceeds
of the International Bioflavonoid Symposium (Munich: Elsevier)
* Bergner P (2002-2003) “Herbs and insulin resistance” Medical Herbalism
13(2):1,3-
Berenguer J, Carrasco D (1977) "Double-blind trial of silymarin versus
placebo in the treatment of chronic hepatitis" Munch Med Wochenschr
119:240-60
* Bingel AS, Farnsworth NR (1994) "Higher plants as potential sources of
galactagogues" Econ Med Plant Res 6:1-54 [review]
Blevins R, Dumic M (1980) "The effect of delta-9-tetrahydrocannabinol on
herpes simplex virus replication" J Gen Virol 49:427-31
Braquet PG, Spinnewyn B, Braquet M, et al. (1985) Blood & Vessel 16:558
Cáceres A, Girón LM, Martínez AM (1987) "Diuretic activity of plants used
for the treatment of urinary ailments in Guatemala" J Ethnopharmacol
19:233-45
Cáceres A, Saravia A, Rizzo S, et al. (1992) "Pharmacologic properties of
Moringa oleifera. 2: Screening for antispasmodic, antiinflammatory and
diuretic activity" J Ethnopharmacol 36:233-7
Cellini L, Di Campli E, Masulli M, et al. (1996) Inhibition of Helicobacter
pylori by garlic extract (Allium sativum)" FEMS Immunol Med Microbiol
13(4):273-7
Chaudhry PS, Cabrera J, Juliani HR, Varma SD (1983) "Inhibition of human
lens aldose reductase by flavonoids, sulindac and indomethacin" Biochem
Pharmacol 32:1995-8
Chen I, McDougal A, Wang F, Safe S (1998) "Aryl hydrocarbon receptor-
mediated antiestrogenic and antitumorigenic activity of diindolylmethane"
Carcinogenesis 19:1631-9
Chiang J, et al. "Three inhibitors of type I human immunodeficiency virus
long terminal repeat-directed gene expression and virus replication" Proc
Natl Acad Sci 1991;90:1839-42
Choi SU, Ryu SY, Yoon SK, et al. (1999) “Effects of flavonoids on the
growth and cell cycle of cancer cells” Anticancer Res 19(6B):5229-33
see abstract at end of monograph
Chu CY, Tsai YY, Wang CJ, et al. (2001) "Induction of apoptosis by
esculetin in human leukemia cells" Eur J Pharmacol 416:25-32](https://image.slidesharecdn.com/boeyarnell-herbactions-110417235042-phpapp02/85/Bo-eyarnell-herbactions-52-320.jpg)
![Actions of Medicinal Plants 53 © 2007 Eric Yarnell, ND
Cooke DW Lallinger GJ Durack DT. In vitro sensitivity of Naegleria
fowleri to qinghaosu and dihydroqinghaosu. J Parasitol (1987 Apr)
73(2):411-3
Davis LE, Shen JK, Cai Y (1990) "Antifungal activity in human cerebrospinal
fluid and plasma after intravenous administration of Allium sativum"
Antimicrob Agents Chemother 34:651-3
* de Carvalho PB, Ferreria EI (2001) "Leishmaniasis phytotherapy. Nature's
leadership against an ancient disease" Fitoterapia 72:599-618 [review]
* Devi BA, Kamalakkannan N, Prince PSM (2003) “Supplementation of fenugreek
leaves to diabetic rats. Effect on carbohydrate metabolic enzymes in
diabetic liver and kidney” Phytother Res 17:1231-3
Dorsch W, Wagner H (1991) "New antiasthmatic drugs from traditional
medicine?" Int Arch Allergy Appl Immunol 94:262-5 [review]
* Elgorashi EE, Stafford GI, van Staden J (2004) “Acetylcholinesterase
enzyme inhibitory effects of Amaryllidaceae alkaloids” Planta Med 70:260-2
Fabry W, Okemo P, Ansorg R (1996) "Activity of east African medicinal
plants against Helicobacter pylori" Chemotherapy 42(5):315-7
Fabry W, Okemo P, Mwatha WE, et al. (1996) "Susceptibility of Helicobacter
pylori and Candida spp. to the east African plant Terminalia spinosa"
Arzneim Forsch 46(5):539-40
* Farzami B, Ahmadvand D, Vardasbi S, et al. (2003) “Induction of insulin
secretion by a component of Urtica dioica leave [sic] extract in perifused
[sic] islets of Langerhans and its in vivo effects in normal and
streptozotocin diabetic rats” J Ethnopharmacol 89:47-53
Ferriola PC, Cody V and Middleton E Jr (1989) "Protein kinase C inhibition
by plant flavonoids. Kinetic mechanisms and structure-activity
relationships" Biochem Pharmacol 38:1617-24
Fitzpatrick M (2000) "Soy formulas and the effects of isoflavones on the
thyroid" N Z Med J 113:24-26 [review]
Fotsis T, Pepper MS, Montesano R, et al. (1998) "Phytoestrogens and
inhibition of angiogenesis" Baillieres Clin Endocrin Metab 12:649-66
Gaitan EO, Cooksey RC (1989) "General concepts of environmental
goitrogenesis" In: Gaitan E (ed) Environmental Goitrogenesis (Boca Raton,
FL: CRC Press):3-11](https://image.slidesharecdn.com/boeyarnell-herbactions-110417235042-phpapp02/85/Bo-eyarnell-herbactions-53-320.jpg)




![Actions of Medicinal Plants 58 © 2007 Eric Yarnell, ND
Nabekura T, Kamiyama S, Kitagawa S (2005) “Effects of dietary
chemopreventive phytochemicals on P-glycoprotein function” Biochem Biophys
Res Commun 327(3):866-70.
see abstract at end of monograph
Nagai T, Suzuki Y, Tomimori T and Yamada H (1995) "Antiviral activity of
plant flavonoid, 5,7,4'-trihydroxy-8-methoxyflavone, from the roots of
Scutellaria baicalensis against influenza A (H3N2) and B viruses" Biol
Pharm Bull 18:295-9
Newton SM, Lau C, Wright CW (2000) "A review of antimycobacterial natural
products" Phytother Res 14:303-22 [review]
Nikaido T, Ohmoto T, Noghuchi H, et al. (1981) "Inhibitors of cyclic AMP
phosphodiesterase in medicinal plants" Planta Med 43:18-23
Nikaido T, Ohmoto T, Sankawa U, et al. (1988) "Inhibition of adenosine
3',5'-cyclic monophosphate phosphodiesterase by flavonoids. II." Chem Pharm
Bull (Tokyo) 36(2):654-61
Nikaido T, Ohmoto T, Kinoshita T, et al. (1989) "Inhibition of adenosine
3',5'-cyclic monophosphate phosphodiesterase by flavonoids. III." Chem
Pharm Bull (Tokyo) 37(5):1392-5
see abstract at end of monograph
Nonaka G-I, Lee K-H, Cheng Y-C and Kilkuskie RE (1990) "Inhibition of human
retroviruses" Patent #WO 90/04968
Nunez D, Chignard M, Korth R, et al. (1986) Eur J Pharmacol 123:197
Nyarko AK, Asare-Anane H, Ofosuhene M, Addy ME (2002) “Extract of Ocimum
canum lowers blood glucose and facilitates insulin release by isolated
pancreatic beta-islet cells” Phytomedicine 9(4):346-51.
Ohmoto T, Aikawa R, Nikaido T, et al. (1986) "Inhibition of adenosine
3',5'-cyclic monophosphate phosphodiesterase by components of Sophora
flavescens Aiton." Chem Pharm Bull (Tokyo) 34(5):2094-9
Ohmoto T, Nikaido T, Koike K, et al. (1988) "Inhibition of adenosine 3',5'-
cyclic monophosphate phosphodiesterase by alkaloids. II." Chem Pharm Bull
(Tokyo) 36(11):4588-92
Oliver-Bever B, Zahnd GR (1979) "Plants with oral hypoglycaemic action" Q J
Crude Drug Res 17:139-96
Otero-R; Nunez-V; Barona-J; et al. (2000) "Snakebites and ethnobotany in
the northwest region of Colombia - Part III: Neutralization of the](https://image.slidesharecdn.com/boeyarnell-herbactions-110417235042-phpapp02/85/Bo-eyarnell-herbactions-58-320.jpg)

![Actions of Medicinal Plants 61 © 2007 Eric Yarnell, ND
Vanden Berghe DA, Vlietinck AJ and Van Hoof L (1986) "Plant products as
potential antiviral agents" Bull Inst Pasteur 101-47
Varma SD (1986) "Inhibition of aldose reductase by flavonoids: Possible
attenuation of diabetic complications" In: Plant Flavonoids in Biology and
Medicine: Biochemical, Pharmacological, and Structure-Activity
Relationships (NY: Alan R. Liss):343-57
Varma SD, Kinoshita JH (1976) "Inhibition of aldose reductase by
flavonoids. Their possible role in the prevention of diabetic cataracts"
Biochem Pharmacol 25:2505-13
* Vasanth S, Gopal RH, Rao RB (1990) "Plant anti-malarial agents" J Sci
Industr Res 49:68-77 [review]
Viana M, Barbas C, Bonet B, et al. (1996) "In vitro effects of a flavonoid-
rich extract on LDL oxidation" Atherosclerosis 123(1-2):83-91
see abstract at end of monograph
Vinitketkumnuen U, Puatanachokchai R, Lertprasertsuke N, et al. (1996)
"Antimutagenicity and anti-tumor activity of lemon grass" Mutat Res Environ
Mutagen 359:200-1
Wacker A, Hilbig W "Virus-inhibition by Echinacea purpurea" Planta Med
1978;33:89-102
Wöhlbling R, Leonhardt K (1994 "Local therapy of herpes simplex with dried
extract from Melissa officinalis" Phytomedicine 1:25-31
Xu HX, Lee SF (2001) "Activity of plant flavonoids against antibiotic-
resistant bacteria" Phytother Res 15(1):39-43
see abstract at end of monograph
Zamora (1984) Cytotoxic, Antimicrobial and Phytochemical Properties of
Larrea tridentata Cav. Doctoral Dissertation. Auburn University, Auburn,
Alabama.
Zhang L, Yang LW, Yang LJ (1992) “[Relation between Helicobacter pylori and
pathogenesis of chronic atrophic gastritis and the research of its
prevention and treatment]” Zhongguo Zhong Xi Yi Jie He Za Zhi 12(9):521-3,
515-6 [Article in Chinese]
Zhou YP, Zhang JP (1989) "Oral baicalin and liquid extract of licorice reduce
sorbitol levels in red blood cell in diabetic rats" Chin Med J 102:203-6
CLX. Abstracts to articles mentioned above](https://image.slidesharecdn.com/boeyarnell-herbactions-110417235042-phpapp02/85/Bo-eyarnell-herbactions-61-320.jpg)



![Actions of Medicinal Plants 65 © 2007 Eric Yarnell, ND
carcinoma KB-C2 cells and the fluorescent P-glycoprotein substrates
daunorubicin and rhodamine 123. The effects of natural chemopreventive
compounds, capsaicin found in chilli peppers, curcumin in turmeric, [6]-
gingerol in ginger, resveratrol in grapes, sulforaphane in broccoli, 6-
methylsulfinyl hexyl isothiocyanate (6-HITC) in Japanese horseradish
wasabi, indole-3-carbinol (I3C) in cabbage, and diallyl sulfide and diallyl
trisulfide in garlic, were examined. The accumulation of daunorubicin in
KB-C2 cells increased in the presence of capsaicin, curcumin, [6]-gingerol,
and resveratrol in a concentration-dependent manner. The accumulation of
rhodamine 123 in KB-C2 cells was also increased, and the efflux of
rhodamine 123 from KB-C2 cells was decreased by these phytochemicals.
Sulforaphane, 6-HITC, I3C, and diallyl sulfide and diallyl trisulfide had
no effect. These results suggest that dietary phytochemicals, such as
capsaicin, curcumin, [6]-gingerol, and resveratrol, have inhibitory effects
on P-glycoprotein and potencies to cause drug-food interactions.
Nikaido, et al. 1989 Abstract: Sixty-one flavanones, twenty-six
isoflavones and eight other flavonoids, obtained from Sophora tomentosa,
S. flavescens, Scutellaria baicalensis and other medicinal plants or
synthesized, were tested for their inhibitory activity against adenosine
3',5'-cyclic monophosphate (cAMP) phosphodiesterase from beef heart. The
structure-activity relationships were investigated.
Otero, et al. 2000 Abstract: Thirty-one of 75 extracts of plants used by
traditional healers for snakebites, had moderate or high neutralizing
ability against the haemorrhagic effect of Bothrops atrox venom from
Antioquia and Choco, north-western Colombia. After preincubation of several
doses of every extract (7.8- 4000 < mu >g/mouse) with six minimum
haemorrhagic doses (10 < mu >g) of venom, 12 of them demonstrated 100%
neutralizing capacity when the mixture was i.d. injected into mice (18-20
g). These were the stem barks of Brownea rosademonte (Caesalpiniaceae) and
Tabebuia rosea (Bignoniaceae); the whole plants of Pleopeltis percussa
(Polypodiaceae), Trichomanes elegans (Hymenophyllaceae) and Senna dariensis
(Caesalpiniaceae); rhizomes of Heliconia curtispatha (Heliconiaceae);
leaves and branches of Bixa orellana (Bixaceae), Philodendron tripartitum
(Araceae), Struthanthus orbicularis (Loranthaceae) and Gonzalagunia
panamensis (Rubiaceae); the ripe fruits of Citrus limon (Rutaceae); leaves,
branches and stem of Ficus nymphaeifolia (Moraceae). Extracts of another 19
species showed moderate neutralization (21-72%) at doses up to 4 mg/mouse,
e.g. the whole plants of Aristolochia grandiflora (Aristolochiaceae),
Columnea kalbreyeriana (Gesneriaceae), Sida acuta (Malvaceae), Selaginella
articulata (Selaginellaceae) and Pseudoelephantopus spicatus (Asteraceae);
rhizomes of Renealmia alpinia (Zingiberaceae); the stem of Strychnos
xinguensis (Loganiaceae); leaves, branches and stems of Hyptis capitata
(Lamiaceae), Ipomoea cairica (Convolvulaceae), Neurolaena lobata
(Asteraceae), Ocimum micranthum (Lamiaceae), Piper pulchrum (Piperaceae),
Siparuna thecaphora (Monimiaceae), Castilla elastica (Moraceae) and
Allamanda cathartica (Apocynaceae); the macerated ripe fruits of Capsicum
frutescens (Solanaceae); the unripe fruits of Crescentia cujete](https://image.slidesharecdn.com/boeyarnell-herbactions-110417235042-phpapp02/85/Bo-eyarnell-herbactions-65-320.jpg)


