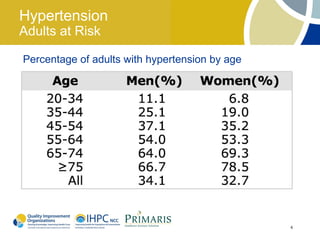
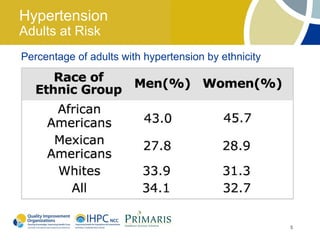
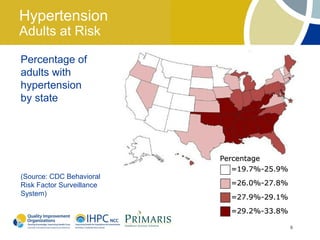
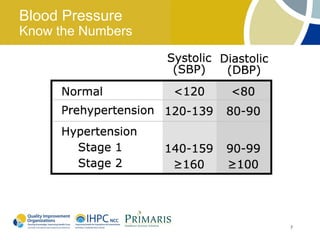
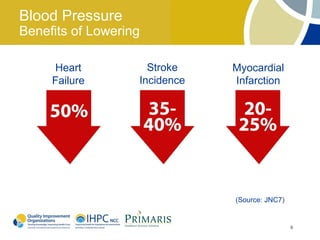
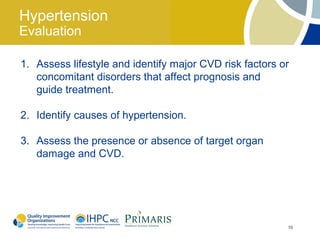
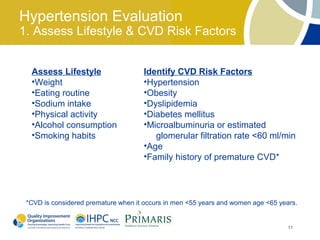
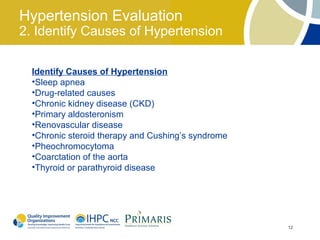
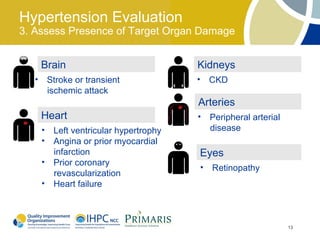
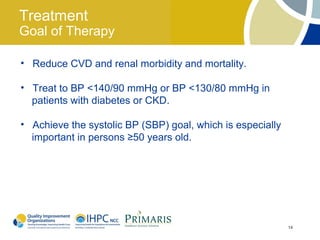
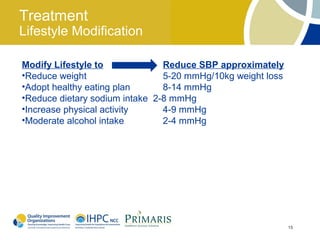
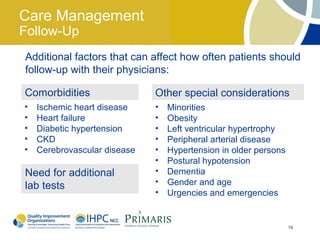
This document provides guidelines for lowering high blood pressure in adults. It outlines that hypertension is very common, affecting 1 in 3 adults in the U.S. It can damage organs like the brain, heart, kidneys, and arteries. The guidelines recommend treating hypertension to a goal of below 140/90 mmHg or 130/80 mmHg for those with diabetes or kidney disease to reduce health risks. Lifestyle changes like losing weight, eating healthy, reducing sodium, and increasing exercise can naturally lower blood pressure. Medications may also be needed to control hypertension. Patients should be regularly monitored until their blood pressure is controlled.