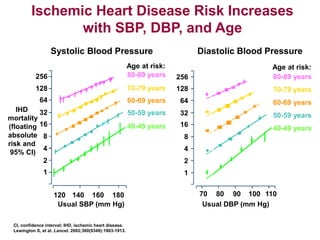
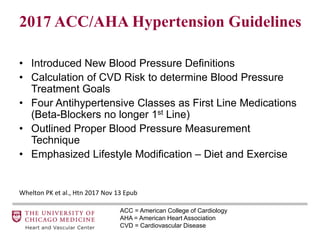
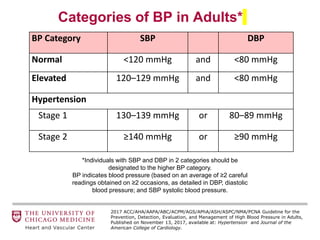
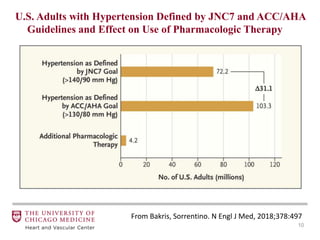
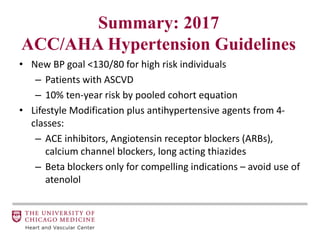
1. The document discusses the 2017 ACC/AHA Hypertension Guidelines, which introduced new definitions for blood pressure categories and recommendations for treatment.
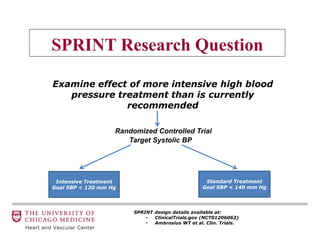
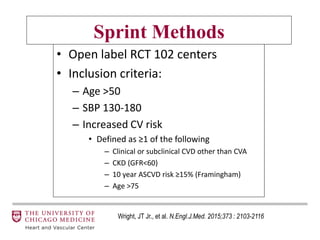
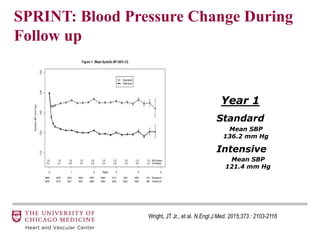
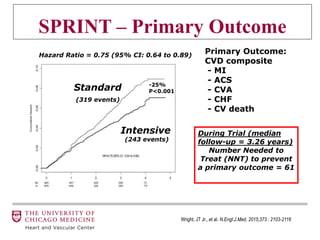
2. It summarizes key findings from the SPRINT trial showing benefits of intensive blood pressure control to below 120/80 mmHg in high-risk individuals.
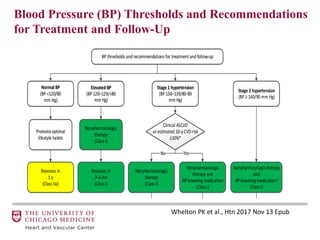
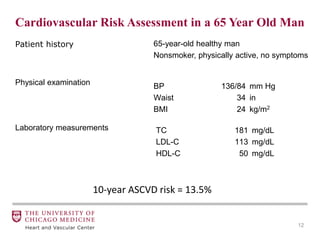
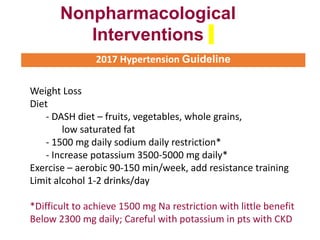
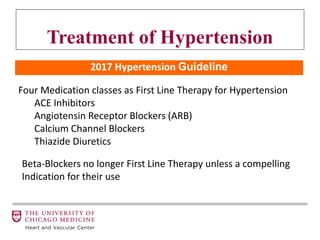
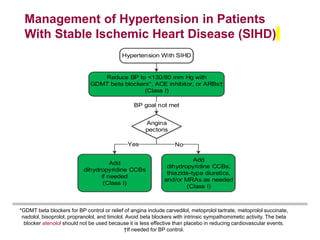
3. The guidelines recommend lifestyle modifications and use of antihypertensive agents from four classes as first-line therapy, with a goal of lowering blood pressure to below 130/80 mmHg in high-risk individuals to reduce cardiovascular events.