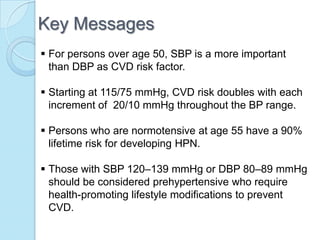
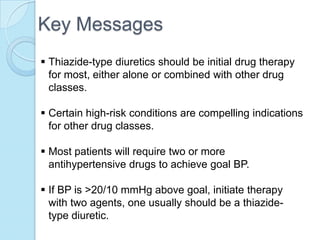
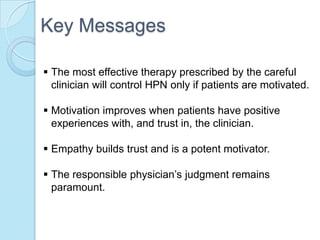
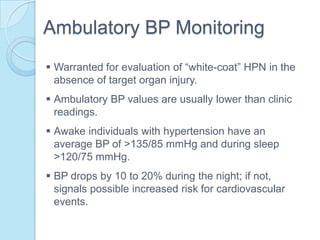
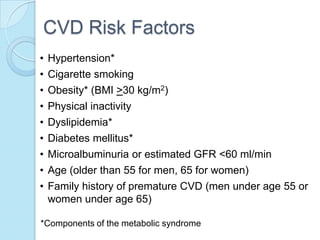
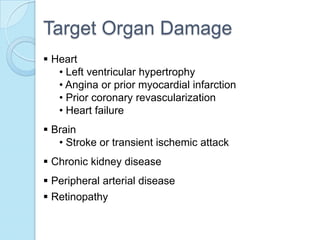
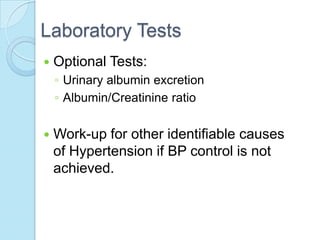
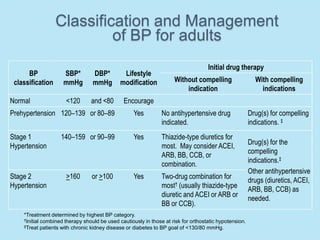
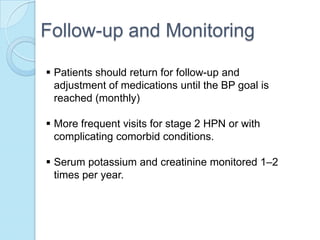
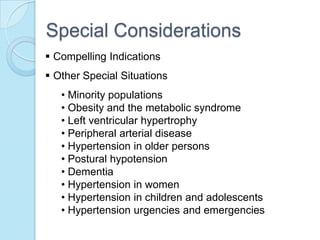
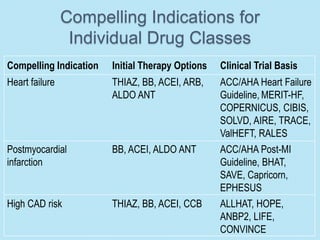
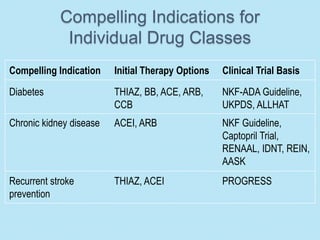
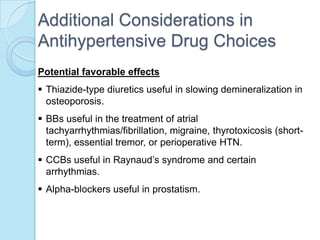
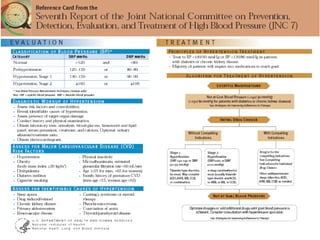
Hypertension is the 5th leading cause of morbidity in the Philippines. This document provides guidelines for diagnosis and treatment of hypertension from the Seventh Report of the Joint National Committee. It defines hypertension as blood pressure over 140/90 mmHg and recommends lifestyle modifications and thiazide diuretics as first-line treatment. Physicians should aim to control blood pressure to under 140/90 mmHg to reduce cardiovascular risks and tailor treatment based on individual patient factors and comorbidities.