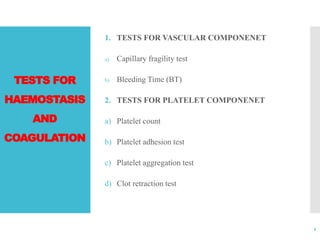
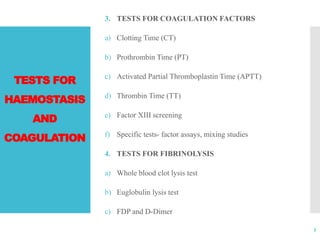
The document outlines various haematology and transfusion medicine tests used to evaluate haemostasis and coagulation, including bleeding time and clotting time tests. It discusses the methods of testing, their procedures, advantages, limitations, and clinical significance related to bleeding and clotting disorders. Specific tests for vascular components, platelet function, coagulation factors, and fibrinolysis are also described.