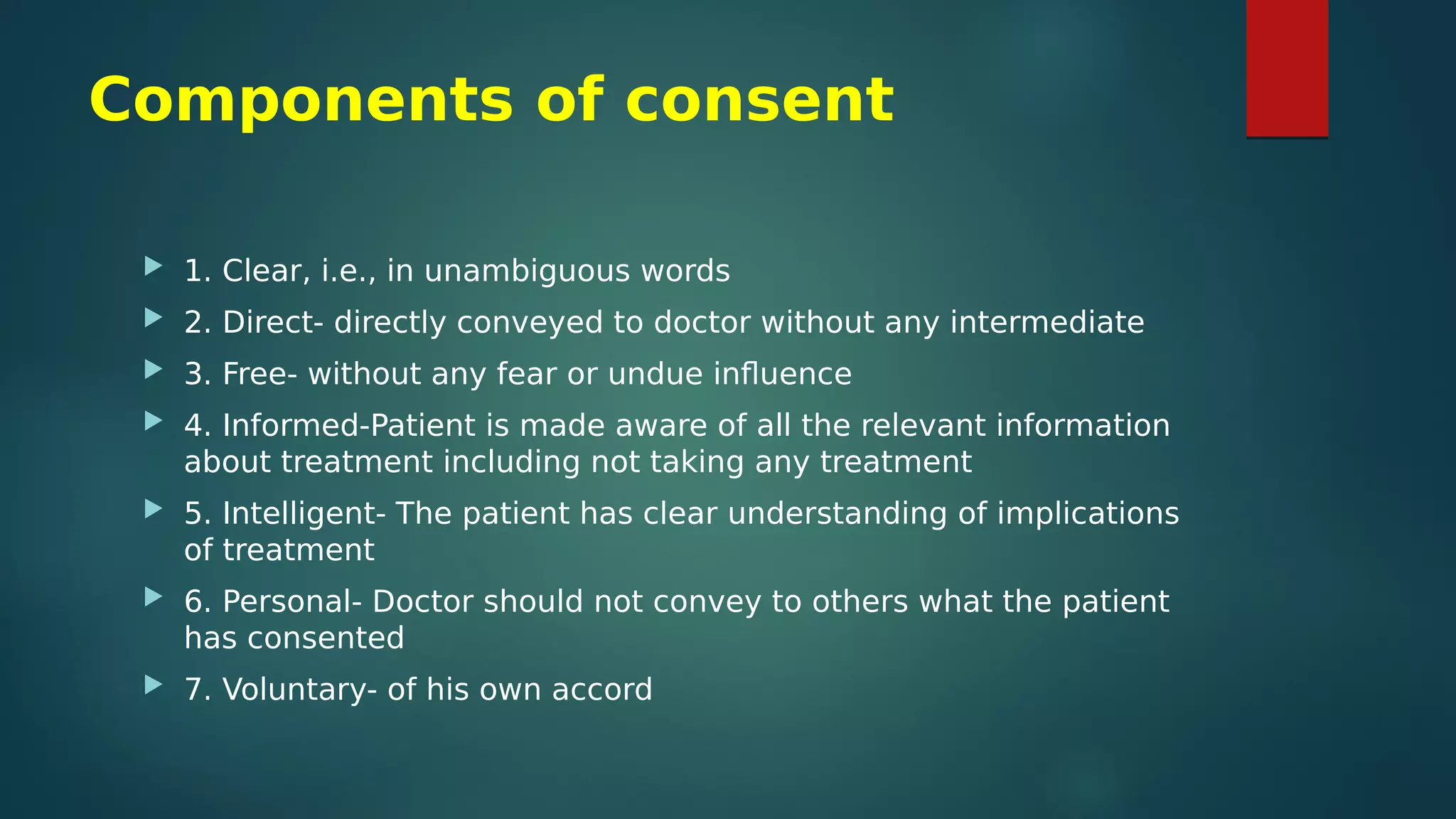
The document discusses the importance of patient autonomy in medical decision-making, emphasizing that physicians should provide all relevant information to allow patients to make informed choices about their treatment. It outlines the legal aspects of consent, including the need for clear, informed, and voluntary agreement from patients before examinations or procedures, with special considerations for gender dynamics. The document also mentions the principle of informed refusal, where patients can decline treatment, and stresses that these decisions must be respected by healthcare providers while ensuring proper documentation to avoid legal repercussions.