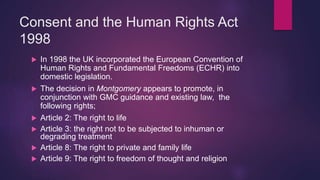
Ed, a 21-year-old Olympic gold medalist, has ruptured his ACL and surgery is offered as treatment. The surgeon explains to Ed that the surgery requires his consent. Consent is grounded in principles of patient autonomy, beneficence, non-maleficence, and justice. For consent to be valid, it must be informed - the patient must understand the nature of the procedure, risks involved, and alternatives. The recent Montgomery ruling established that doctors must take reasonable care to ensure patients understand any material risks or reasonable alternatives.


![Acting Without Consent
Criminal charges could consist of Assault, Actual
Bodily Harm or even Grievous Bodily Harm.
The difficulty with criminal prosecution is that often
actions are not done through malice and as such
criminal charges are rare.
Civil actions are the more common in this area of tort
law, usually through Trespass Against the Person
(Battery) or Negligence.
Civil actions are inter-part disputes; eg: Doctor V
Patient or Nurse V Patient. E.g. Ms B [2002]](https://image.slidesharecdn.com/autonomyconsent-160307141151/85/Autonomy-and-Consent-12-320.jpg)

![Tort of Battery
A claimant can bring a claim of Battery against a healthcare
professional if they fail to comply with the consent of a patient
or act without that patient’s consent.
Consider;
A patient expresses a wish to be cannulated in her right arm
but is instead cannulated in her left arm.
Wrong site surgery (also actionable in negligence)
A doctor who discovered that his patient’s womb was ruptured
whilst performing minor gynaecological surgery performed a
sterilisation without her consent. Devi v West Midlands AHA
[1980]
Ms B [2002].](https://image.slidesharecdn.com/autonomyconsent-160307141151/85/Autonomy-and-Consent-19-320.jpg)
![How Much Information Is Enough?
There is no legal framework that states exactly what facts and
specific information should be given.
The starting point was in Chatterton v Green [1981]. The court
held that consent was valid if the patient had been told in
broad terms about the nature of the procedure.
Traditionally and predominantly the law operated a
“professional standard” approach, i.e. the standard to which it
is the practice for the profession to offer. This approach was
very medically paternalistic- Doctor knows best!](https://image.slidesharecdn.com/autonomyconsent-160307141151/85/Autonomy-and-Consent-21-320.jpg)
![Professional Standard Approach
The Bolam test:
Bolam v Friern Hospital Management Committee
[1957]
“A doctor is not guilty of negligence if he has acted in
accordance with a practice accepted as proper by a
responsible body of medical men skilled in that
particular art.”
In other words a doctor of the same training can avoid
liability if another doctor stands up in court and states
that the actions of the defendant were reasonable.](https://image.slidesharecdn.com/autonomyconsent-160307141151/85/Autonomy-and-Consent-22-320.jpg)
![-Modified in Bolitho v City and Hackney HA
[1997]
Where there is more than one opinion, the
court is entitled to take a logical analysis in
deciding the most appropriate.](https://image.slidesharecdn.com/autonomyconsent-160307141151/85/Autonomy-and-Consent-23-320.jpg)
![What Was Insufficient?
For a patient to be successful in a claim of
negligence or battery as a result of lack of
information, they have to demonstrate that they were
not given such information.
In Chester v Afshar [2002] the Court of Appeal held
that the phrase;
“ I’ve done hundreds of these and I haven’t crippled
anyone yet” fell way beyond the legal and professional
standards.](https://image.slidesharecdn.com/autonomyconsent-160307141151/85/Autonomy-and-Consent-24-320.jpg)