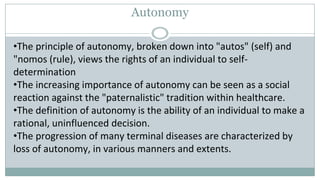
Mrs. Mythili is a 78-year-old widow who was brought to the emergency room by her caretaker with fever and shortness of breath. She had previously expressed to her doctor that she did not want invasive life-sustaining treatments like intubation if she became seriously ill. However, the emergency room intubated her upon finding hypoxia and pneumonia on her chest x-ray. Her doctor must now determine the best course of action that respects both her medical needs and prior expression of autonomy on end-of-life care.