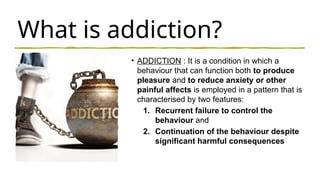
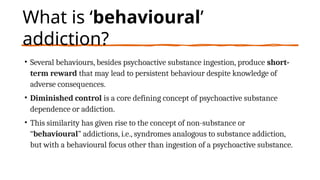
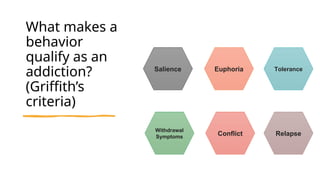
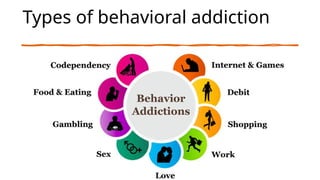
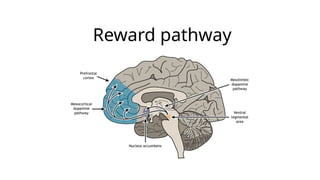
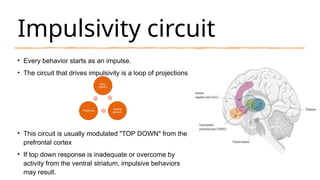
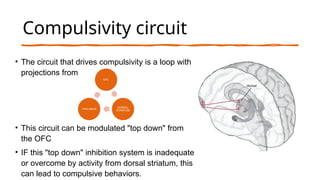
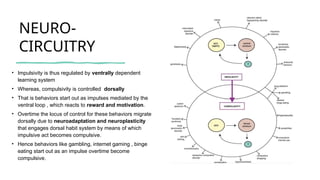
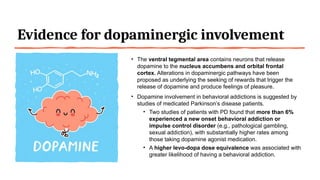
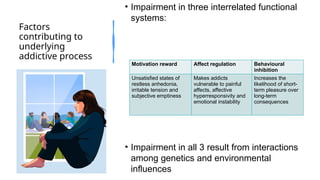
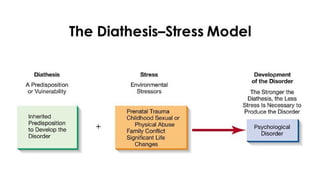
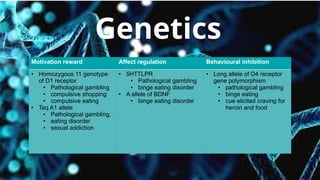
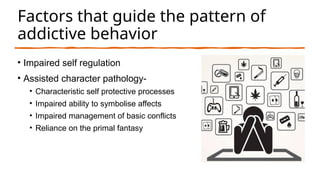
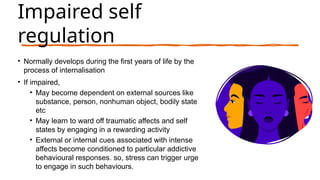
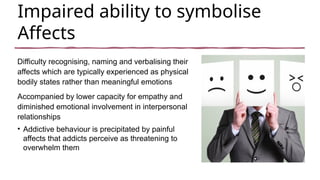
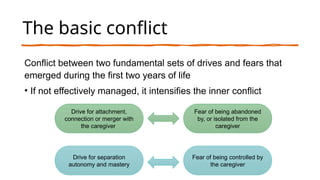
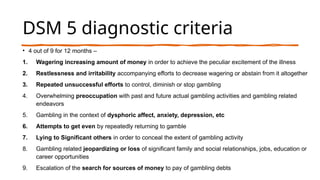
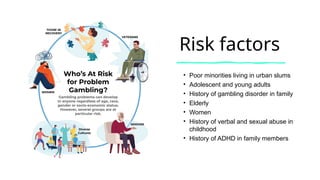
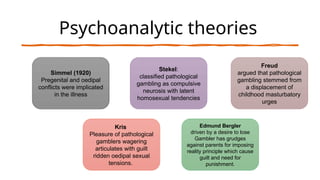
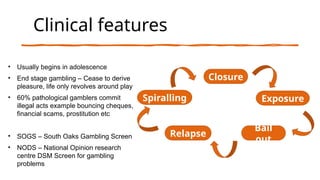
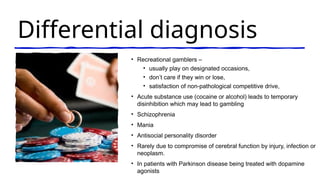
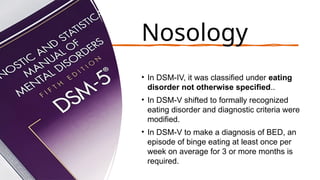
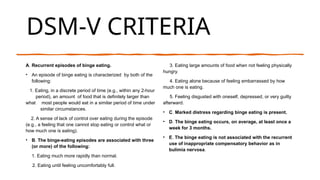
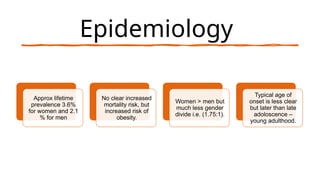
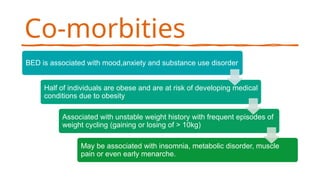
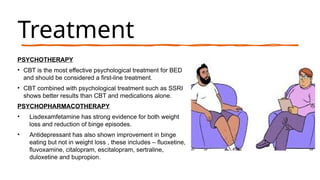
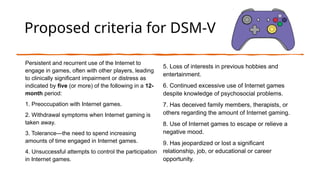
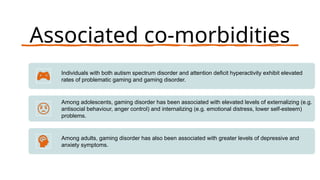
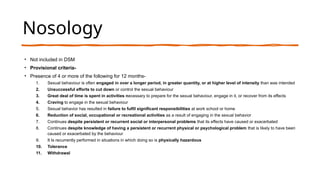
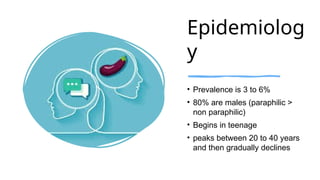
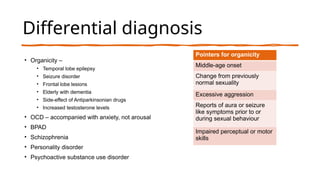
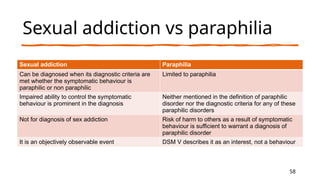
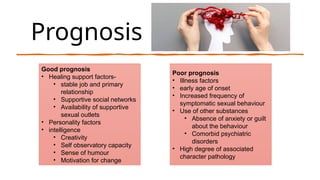
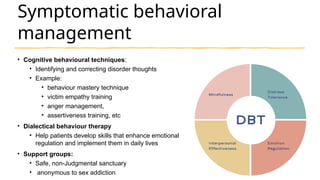
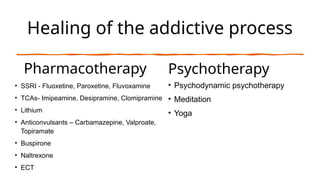
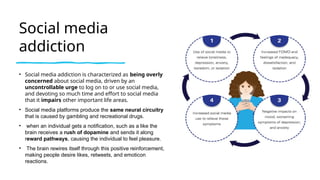
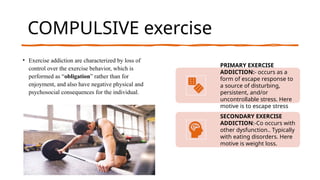
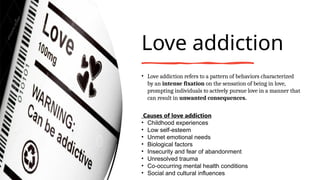
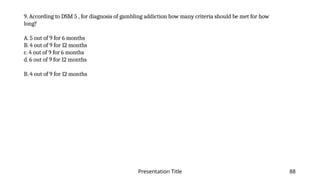
The document discusses behavioral addictions, detailing their definition, neurobiology, and specific disorders such as gambling, binge eating, internet gaming, and sexual addiction. It outlines the criteria for diagnosing these conditions, the underlying neurobiological mechanisms, and various contributing factors, including genetics and environmental aspects. The document emphasizes the need for further research and acknowledges existing treatments while stressing the importance of addressing both psychological and behavioral components of these addictions.