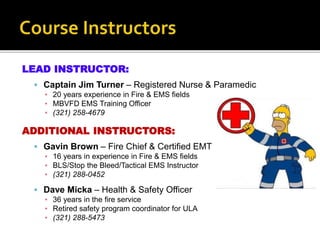
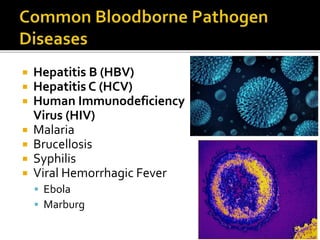
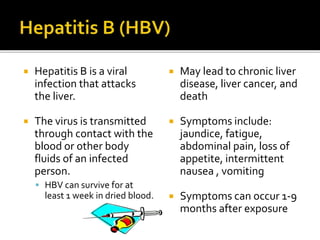
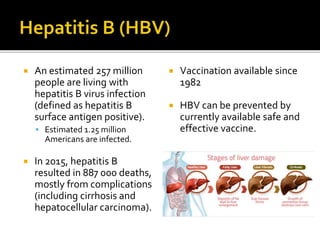
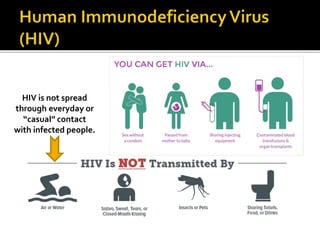
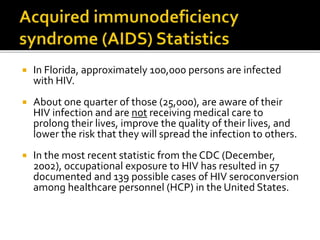
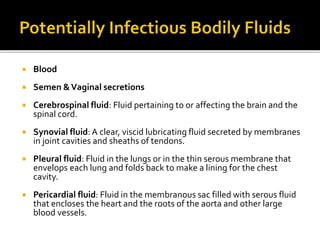
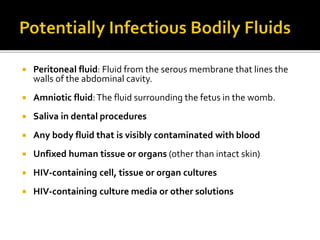
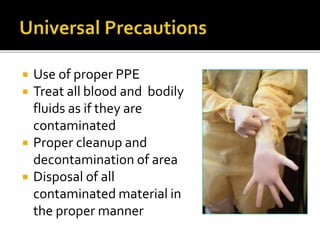
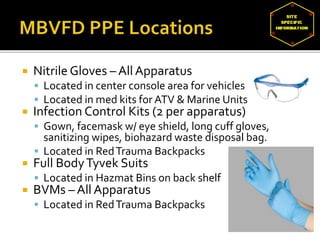
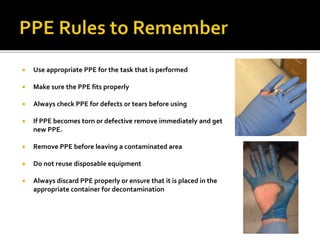
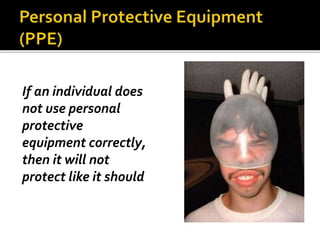
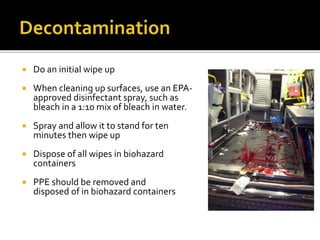
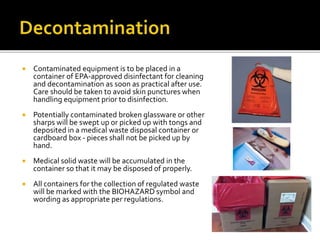
This document provides information and instructions for bloodborne pathogen training. It lists lead instructors and their contact information. It discusses bloodborne pathogens like HIV, hepatitis B, and hepatitis C. It covers topics like standard precautions, modes of transmission, personal protective equipment, cleaning procedures after exposures, and what to do if an exposure occurs. The goal is to educate personnel on preventing exposures to bloodborne diseases and properly responding to any incidents.