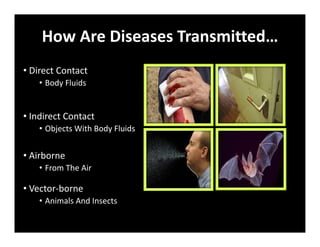
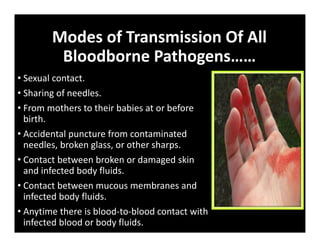
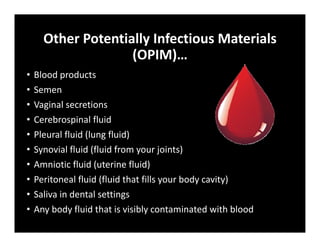
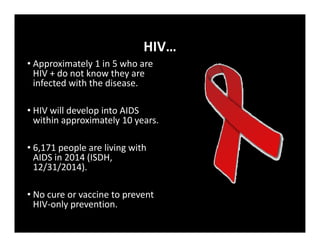
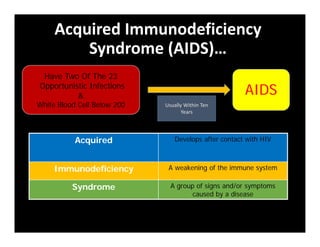
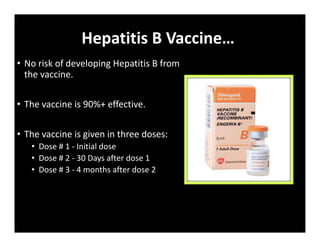
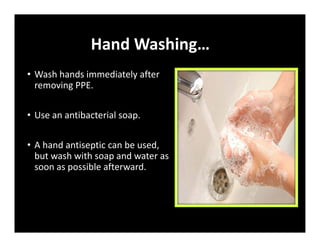
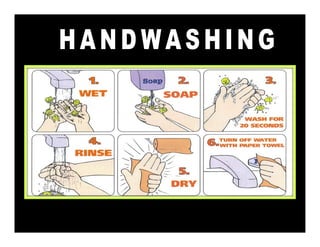
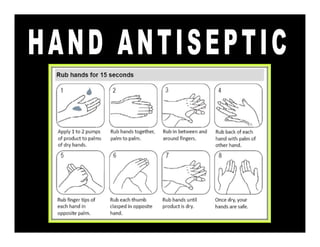
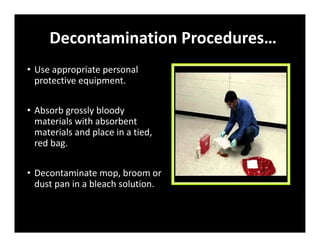
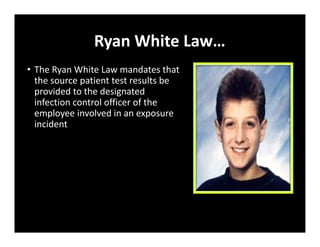
The document outlines the essential information regarding bloodborne pathogens, including their transmission, exposure risks, and universal precautions. It highlights the importance of protective measures, such as personal protective equipment (PPE), reporting procedures for exposures, and the development of an exposure plan. Key pathogens discussed include Hepatitis B, Hepatitis C, and HIV, emphasizing the need for preventive measures and education for at-risk individuals.