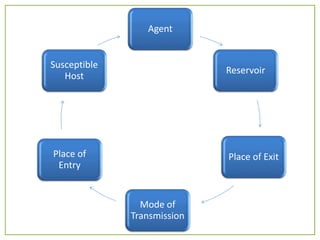
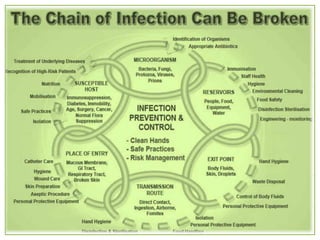
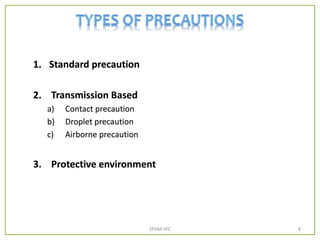
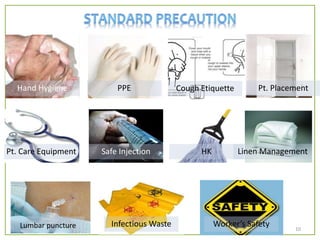
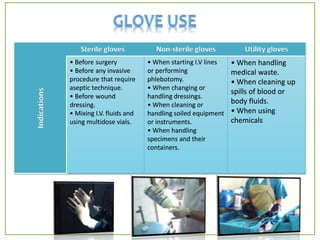
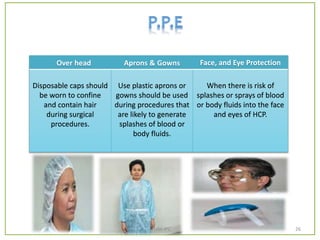
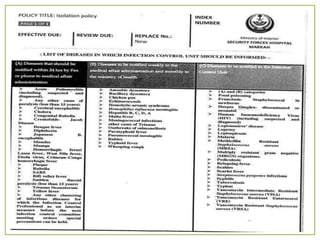
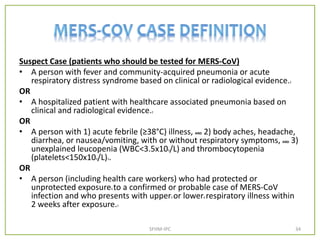
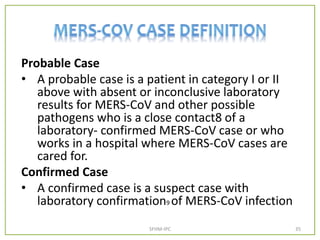
The document outlines infection prevention and control (IPC) guidelines from the Ministry of Interior Security Forces Hospital in Makkah, emphasizing the chain of infection and methods to break it. It covers hand hygiene practices, the use of personal protective equipment (PPE), and precautions for various transmission modes, including standard and transmission-based precautions. Additionally, the document discusses the handling of biological spills, medical waste, and protocols for dealing with suspected viral infections.










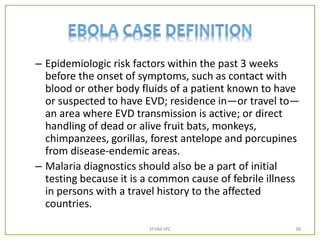
![Suspected Case
• Illness in a person who has both consistent
symptoms and risk factors as follows:
– Clinical criteria, which includes fever of greater than
38.6 C, and additional symptoms such as severe
headache, muscle pain, vomiting, diarrhea,
abdominal pain, or unexplained hemorrhage
(gingival, nasal, cutaneous [petechiae, bruises,
ecchymosis], gastrointestinal, rectal [gross or occult
blood], urinary [gross or microscopic hematuria],
vaginal, or puncture sites bleeding); AND
SFHM-IPC 37](https://image.slidesharecdn.com/staffinduction-1-161214083612/85/Basics-of-the-IPC-practices-37-320.jpg)