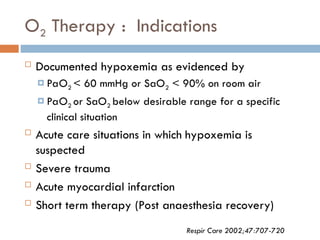
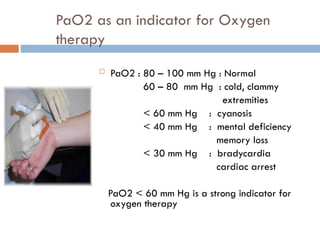
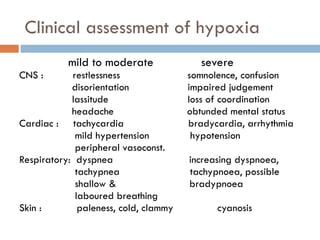
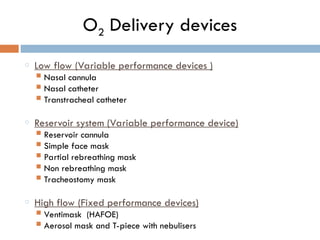
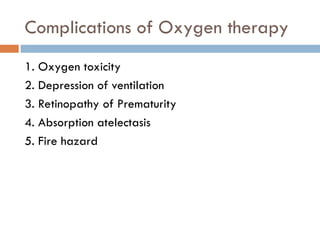
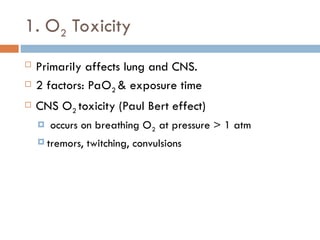
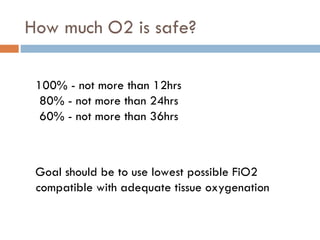
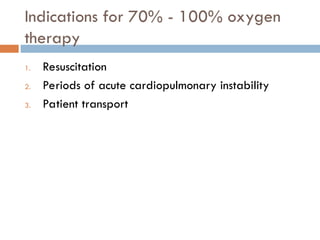
The document discusses oxygen therapy, focusing on its goals, indications, delivery systems, and potential complications. Key objectives include correcting hypoxemia and reducing cardiopulmonary workload, while monitoring indicators like PaO2 and SpO2 for assessment. Complications such as oxygen toxicity and fire hazards must be managed to ensure beneficial use of oxygen as a therapeutic agent.