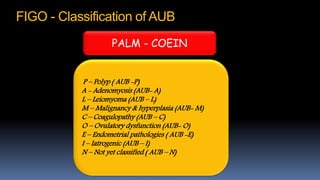
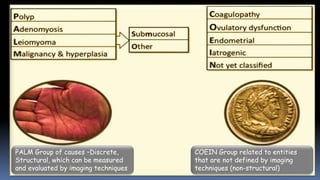
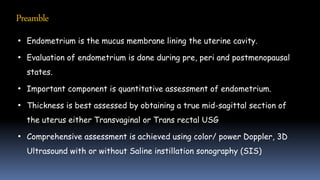
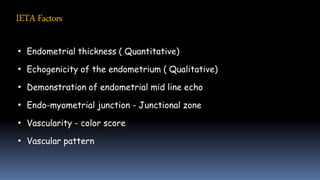
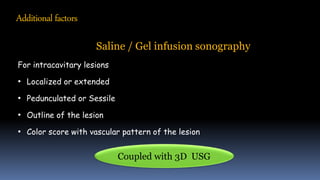
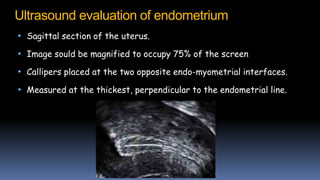
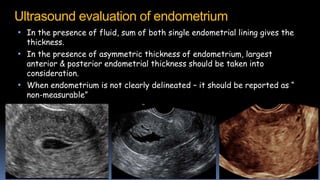
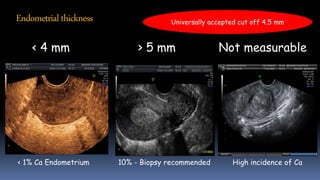
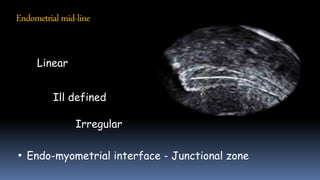
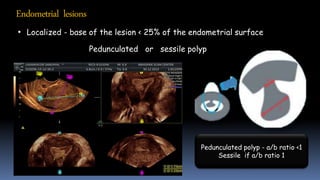
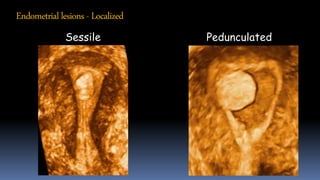
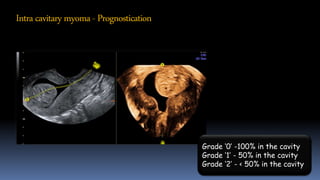
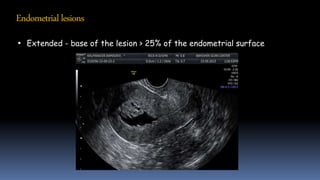
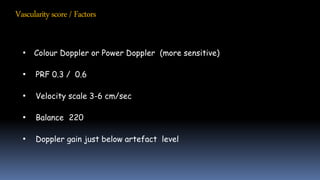
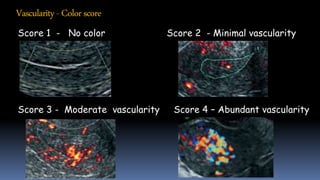
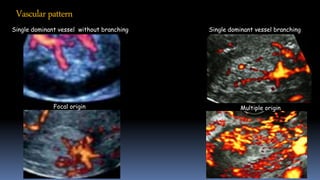
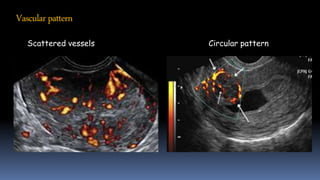
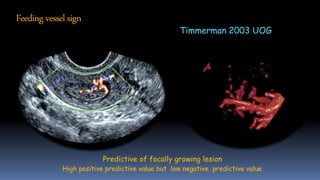
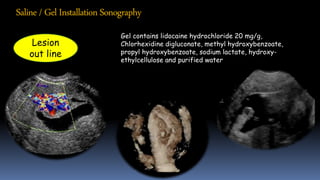
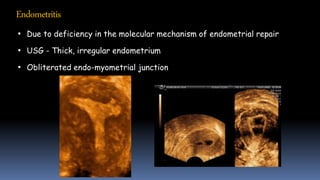
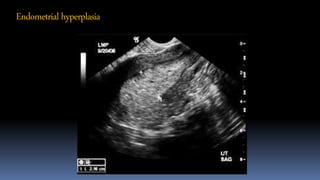
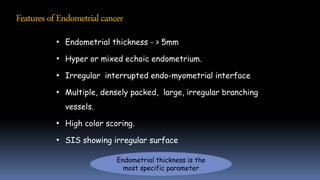
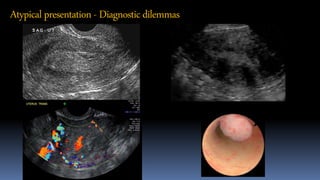
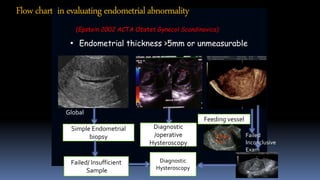
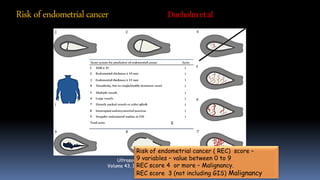
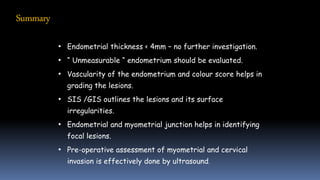
Abnormal uterine bleeding is evaluated using various ultrasound techniques and parameters according to the IETA model. Transvaginal ultrasound is used to measure endometrial thickness and assess echogenicity, vascularity, and the endo-myometrial junction. Additional techniques like saline infusion sonography can outline intracavitary lesions in more detail. Precise ultrasound evaluation and scoring systems can detect endometrial abnormalities and help determine the risk of endometrial cancer. Following guidelines and algorithms helps manage patients and determine if further testing or procedures are needed.