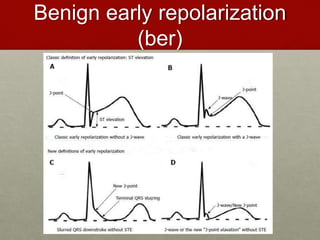
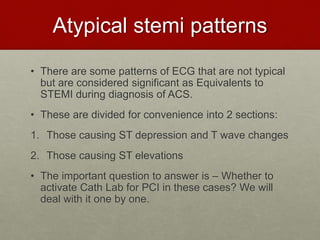
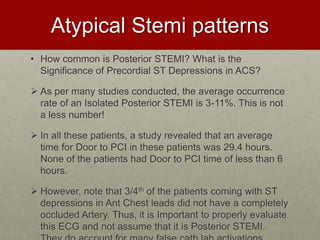
The document discusses atypical STEMI patterns and their equivalents, emphasizing the importance of recognizing these patterns for timely intervention in acute coronary syndrome (ACS). It outlines various ECG features indicative of atypical STEMI such as isolated posterior STEMI, st elevation in aVR, and hyperacute T waves, highlighting criteria for emergency catheter lab activation. The document stresses the need for proper ECG evaluation to differentiate between benign early repolarization and STEMI to avoid delays in treatment.
![Atypical Stemi patterns
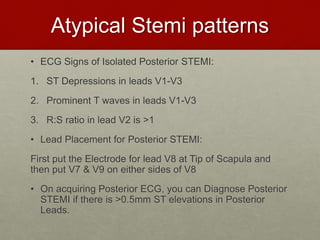
I] Isolated Posterior STEMI:
Posterior heart is involved in 20% cases, but
Isolated Posterior STEMI is seen in 5% patients
only.
When to suspect Posterior STEMI?
1. When there is presence of Inferior & Lateral
STEMI, always do a Posterior ECG to rule out
Posterior STEMI.
2. ECG shows: Isolated ST Depressions in V1-V3](https://image.slidesharecdn.com/atypicalstemipatternsstemiequivalents-200917090851/85/Atypical-stemi-patterns-and-stemi-equivalents-11-320.jpg)
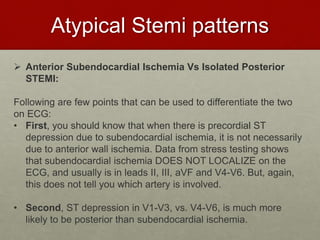
![Atypical Stemi patterns
II] Isolated ST depressions in aVL:
• ST depressions in aVL can be reciprocal to Inferior STEMI.
• Birbaum and Smith demonstrated in a study that Reciprocal ST
Depression in aVL can be apparent in absence of STEMI in
Inferior leads.
• In their study, they noted that 99% of patients with Inferior
STEMI have ST depressions in lead aVL as reciprocal
changes, 93% of which had prominent ST elevations in inferior
leads of >1mm. But 7% of patients had only Isolated ST
depressions in lead aVL, for which on further evaluation noted
that patient had Biomarker positive Inferior STEMI.
• As such, the evidence to prove this Hypothesis is still lacking
and Smith et al are still gathering enough evidence to prove it.
• As of now, this finding in ECG does not need immediate Cath
lab activation for PCI, but an Early Cardiologist consult is a
must.](https://image.slidesharecdn.com/atypicalstemipatternsstemiequivalents-200917090851/85/Atypical-stemi-patterns-and-stemi-equivalents-22-320.jpg)
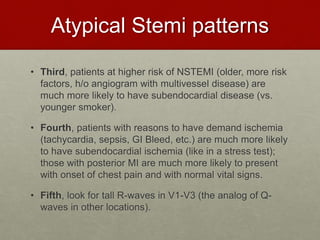
![Atypical Stemi patterns
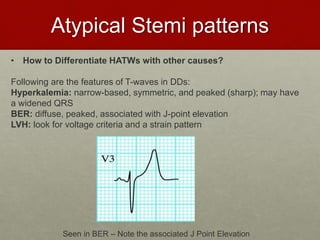
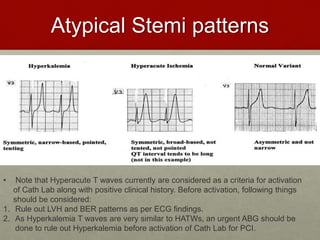
III] Hyperacute T waves:
• Hyperacute T waves are a well defined ECG feature of Early
STEMI. They are noted anywhere between 5 min to 30 min of
onset of Chest Pain.
• They tend to be broad-based, taller than normal T-waves (>5-
10mm in precordial leads) and may be symmetric or asymmetric.
• Very often, reciprocal ST changes are seen in Inferior leads along
with Tall T waves.
• Possible common DD for Tall T waves:
1. Hyperkalemia
2. LVH
3. Benign Early Repolarization
4. Hyperacute Anterior STEMI](https://image.slidesharecdn.com/atypicalstemipatternsstemiequivalents-200917090851/85/Atypical-stemi-patterns-and-stemi-equivalents-23-320.jpg)
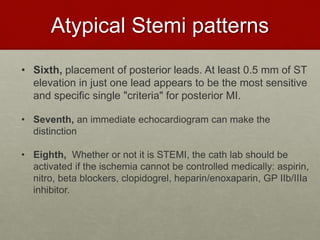
![Atypical Stemi patterns
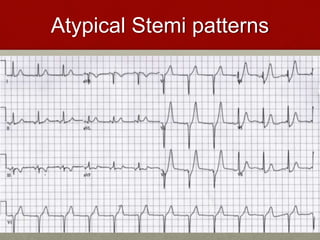
IV] De-Winter’s Pattern:
• In 2008, De-Winter in a Dutch Registry, described a
pattern seen in ECG consistent with Anterior STEMI
and further complete occlusion in LAD found in CAG
in 2% of patients.
• De-Winter’s Pattern: Upsloping ST elevations in
aVR (>1mm) with ST-Depressions and tall T
waves in Precordial leads.](https://image.slidesharecdn.com/atypicalstemipatternsstemiequivalents-200917090851/85/Atypical-stemi-patterns-and-stemi-equivalents-26-320.jpg)

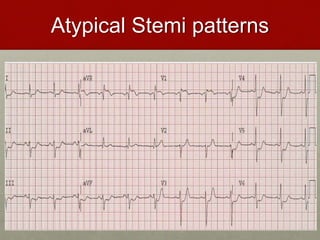
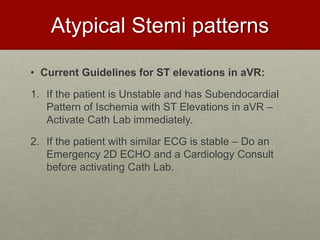
![Atypical Stemi patterns
V] ST elevations in aVR:
• Diffused ST depressions with ST elevations in aVR are
indicative of Subendocardial Ischemia and it indicates
that patient may have one of the following:
1. LMCA occlusion
2. LMEQ Disease (Significant stenosis in LAD and LCX)
3. Triple Vessel Disease
• Although studies have suggested that ST Elevations in
aVR have shown complete LMCA occlusion on CAG, still
the contradictory studies hamper the activation of Cath
Lab for such patients](https://image.slidesharecdn.com/atypicalstemipatternsstemiequivalents-200917090851/85/Atypical-stemi-patterns-and-stemi-equivalents-29-320.jpg)
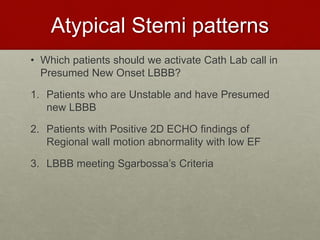
![Atypical Stemi patterns
V] Presumed New LBBB:
• Historically, it is clear that a new onset LBBB is
considered as a STEMI Equivalent.
• But, Studies by Chang et al in 2009 and Neeland et al in
2012 indicated that only about 40% of patients with New
Presumed LBBB have been found to have culprit lesion
on CAG.
• STEMI guidelines from 2013 have now removed
Presumed New LBBB as being Diagnostic for MI “In
Isolation”
• Further, a Presumed New onset LBBB might not be a
New onset LBBB and paperwork drawback may cause
problems.
• Thus, Presumed New Onset LBBB is not an indication for
Cath Lab Activation.](https://image.slidesharecdn.com/atypicalstemipatternsstemiequivalents-200917090851/85/Atypical-stemi-patterns-and-stemi-equivalents-32-320.jpg)
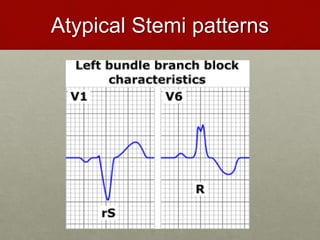
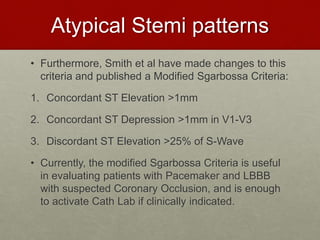
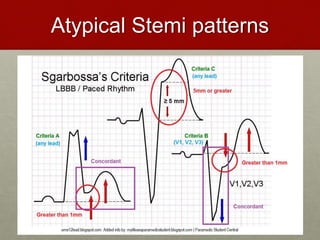
![Atypical Stemi patterns
VI] STEMI Equivalents in Paced Rhythms & Old LBBB:
• Most of the Pacemakers are inserted in Right Ventricle
and the pattern thus formed bypasses the Bundle of His,
ultimately mimicking LBBB pattern.
• Largest study till date for this has been published by
Sgarbossa et al in 32 patients with Pacemaker and
Coronary Occlusion.
• Sgarbossa Criteria: It states that LBBB or Pacemaker
with following signs on ECG are indicative of Coronary
Occlusion-
1. Concordant ST Elevation >1mm
2. Concordant ST Depression >1mm in V1-V3
3. Discordant ST Elevation >5mm](https://image.slidesharecdn.com/atypicalstemipatternsstemiequivalents-200917090851/85/Atypical-stemi-patterns-and-stemi-equivalents-35-320.jpg)