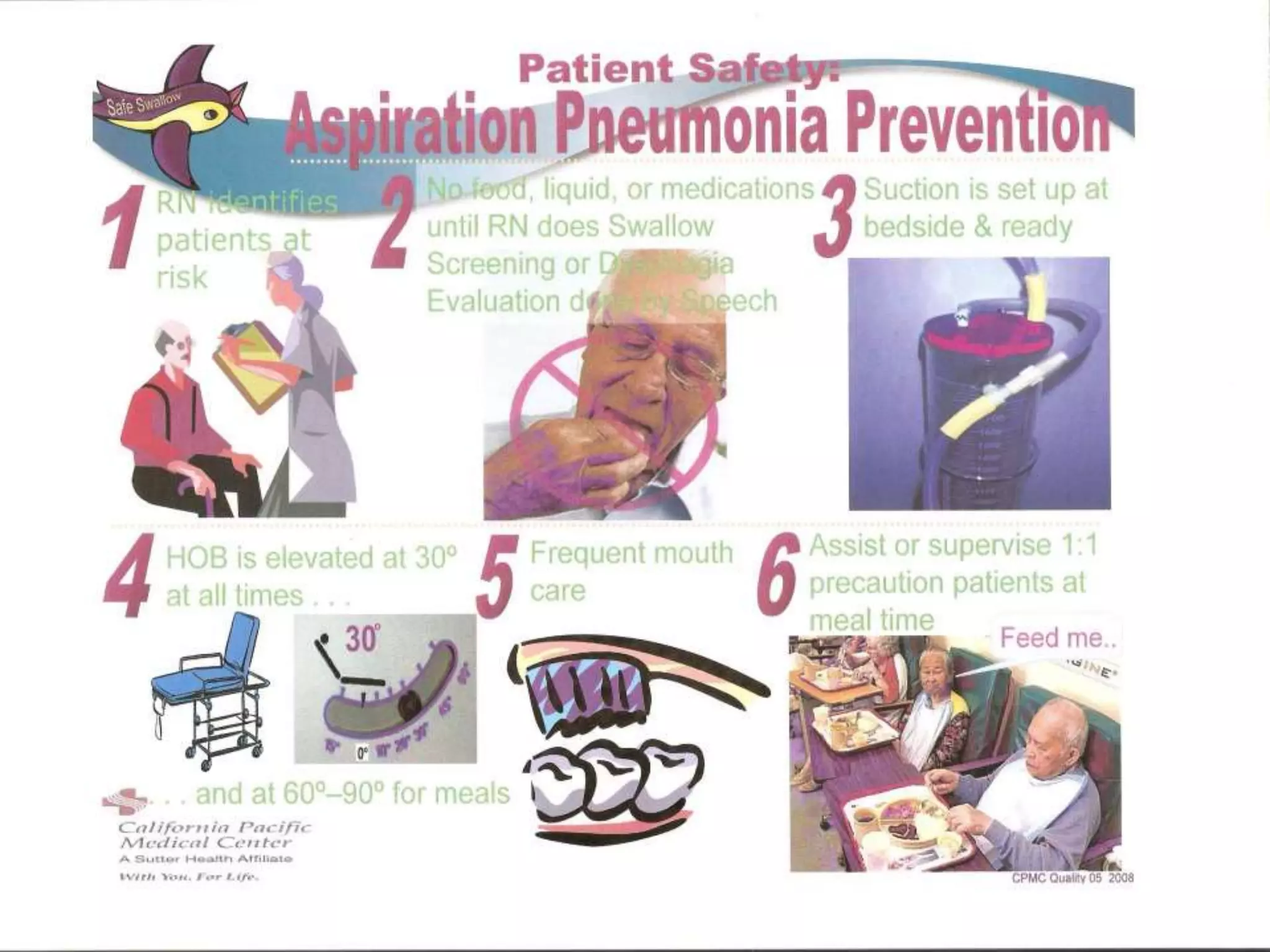
The document discusses aspiration as the inhalation of foreign materials into the trachea and lungs, highlighting the risks and preventive measures for aspiration pneumonia in at-risk patients. It outlines factors increasing aspiration risk, signs and symptoms to observe, and a multidisciplinary approach for assessment and intervention, including guidelines for mealtime practices and the use of feeding tubes. Lastly, it emphasizes the need for proper training for caregivers and includes a care bundle to systematically address aspiration risks.