The document describes an arteriovenous malformation (AVM) in a 22-year-old male patient. Key details include:
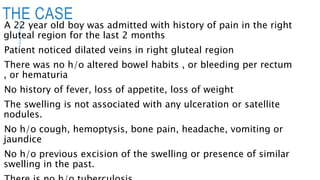
- The patient presented with pain in his right gluteal region and noticed dilated veins. Imaging showed a large AVM in the right gluteal region fed by branches of the right internal iliac artery and draining into the right internal iliac vein.
- The patient underwent embolization to reduce blood flow by 95% prior to planned excision of the AVM.
- AVMs result from an error in vascular development and cause direct shunting of blood from arteries to veins without an intervening capillary bed. Management options aim to alleviate symptoms