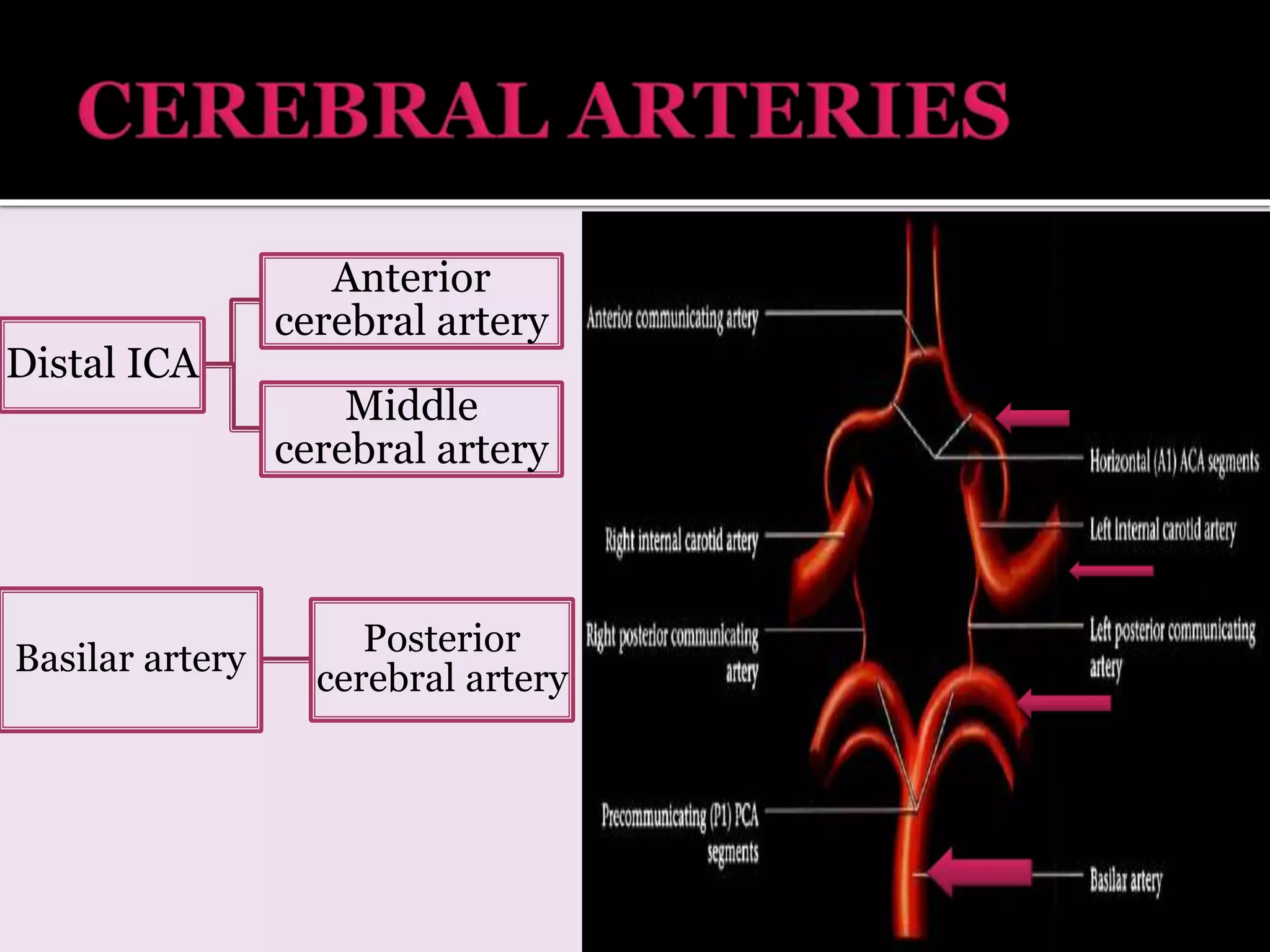
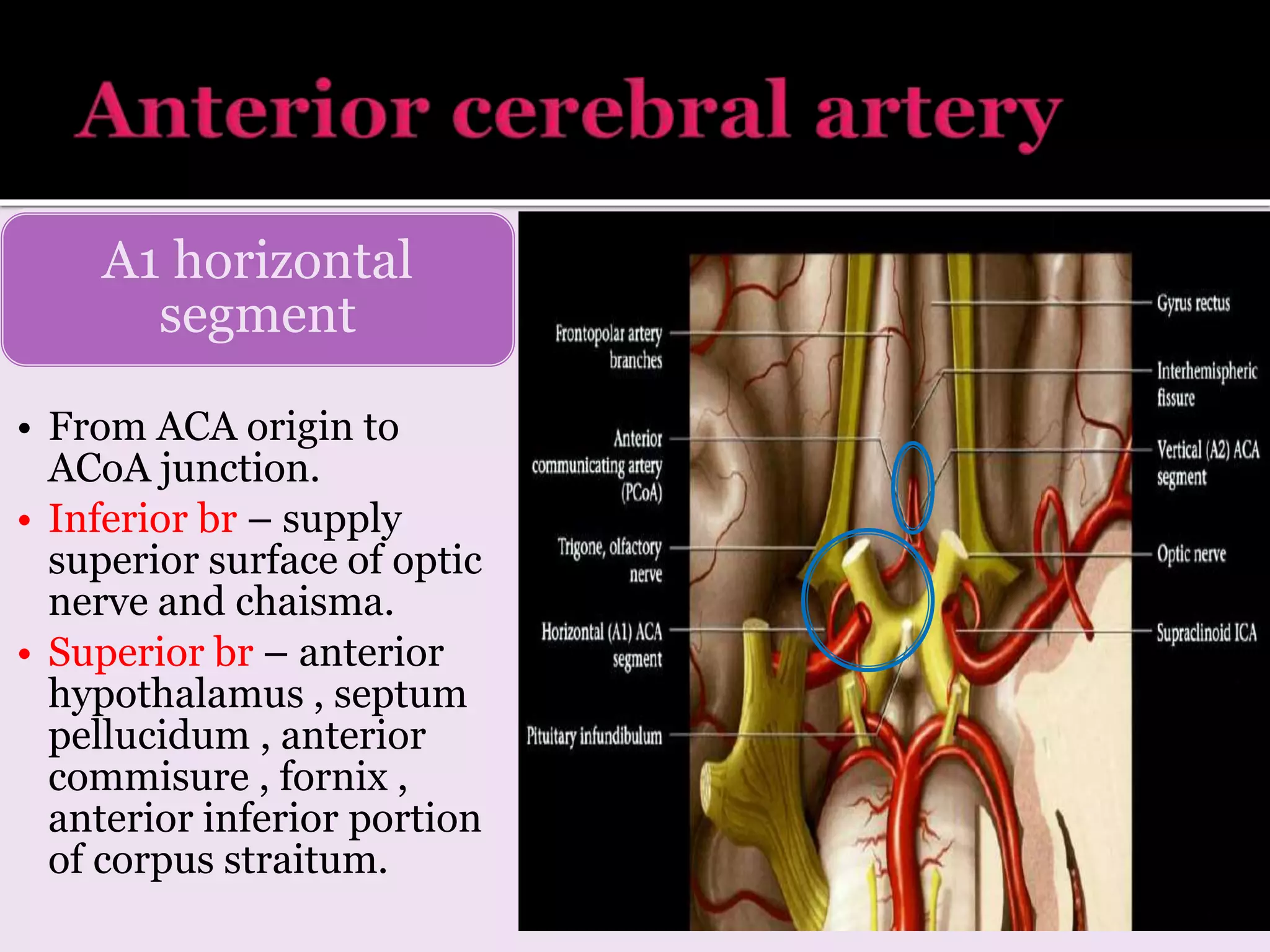
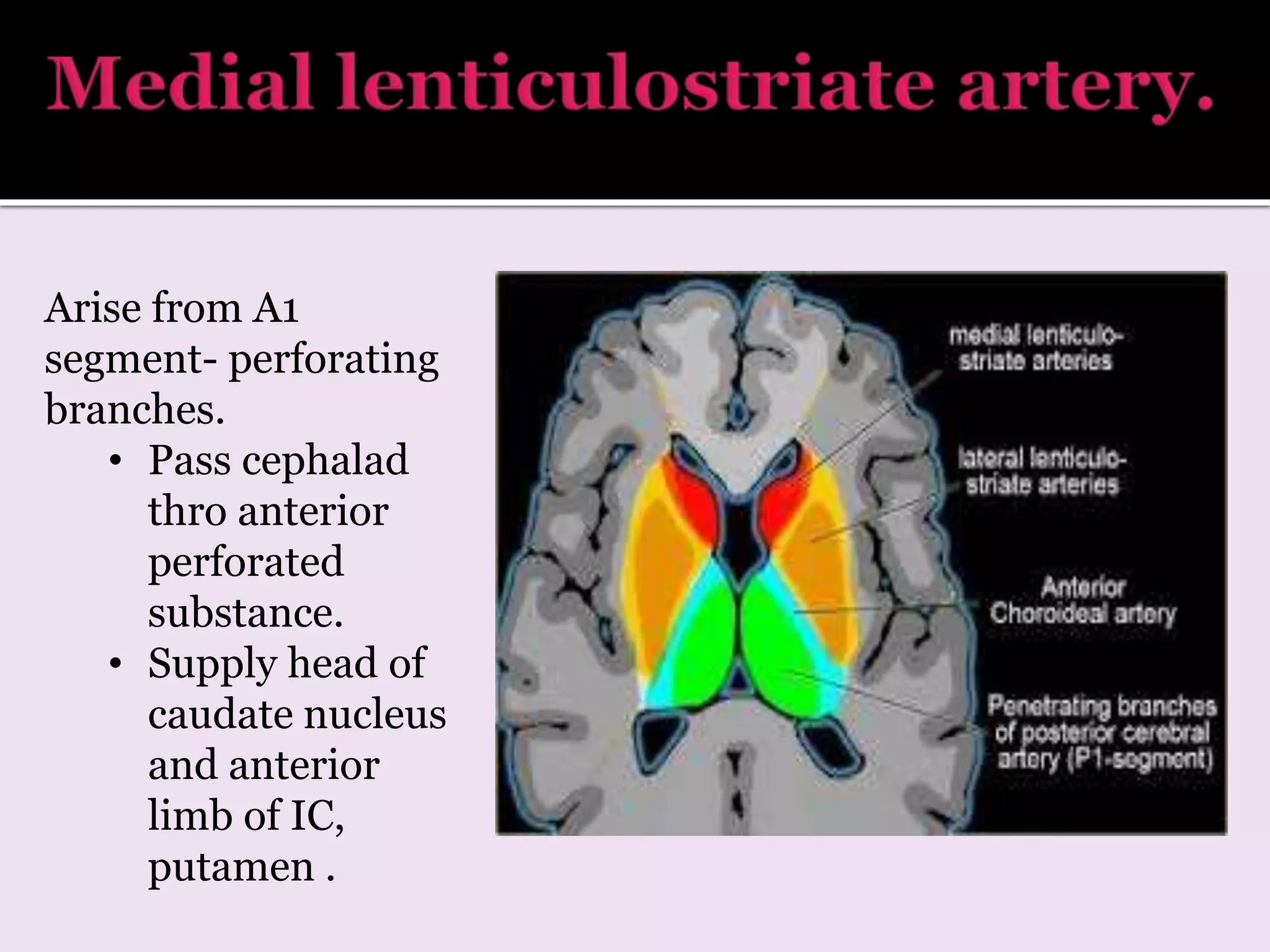
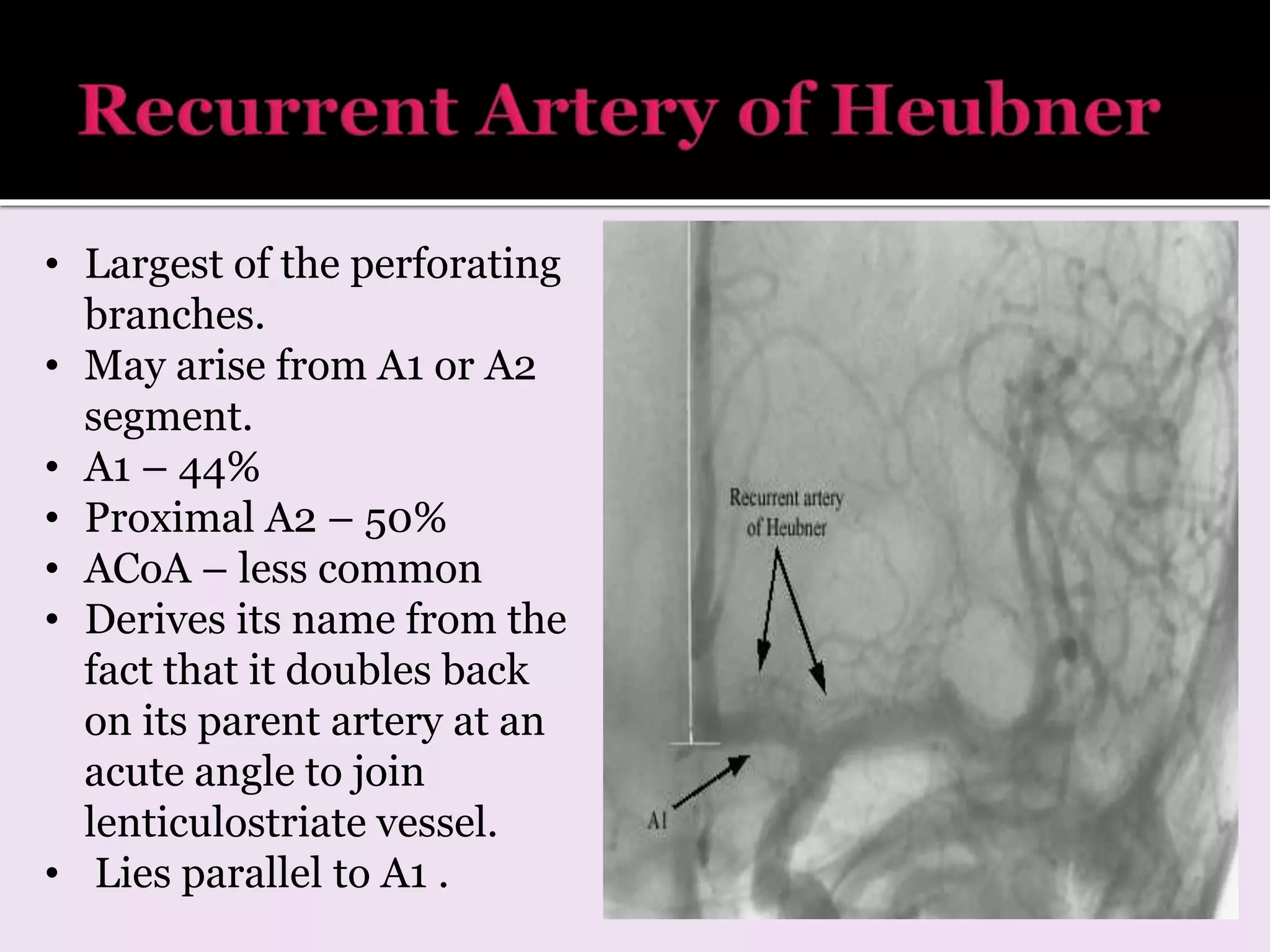
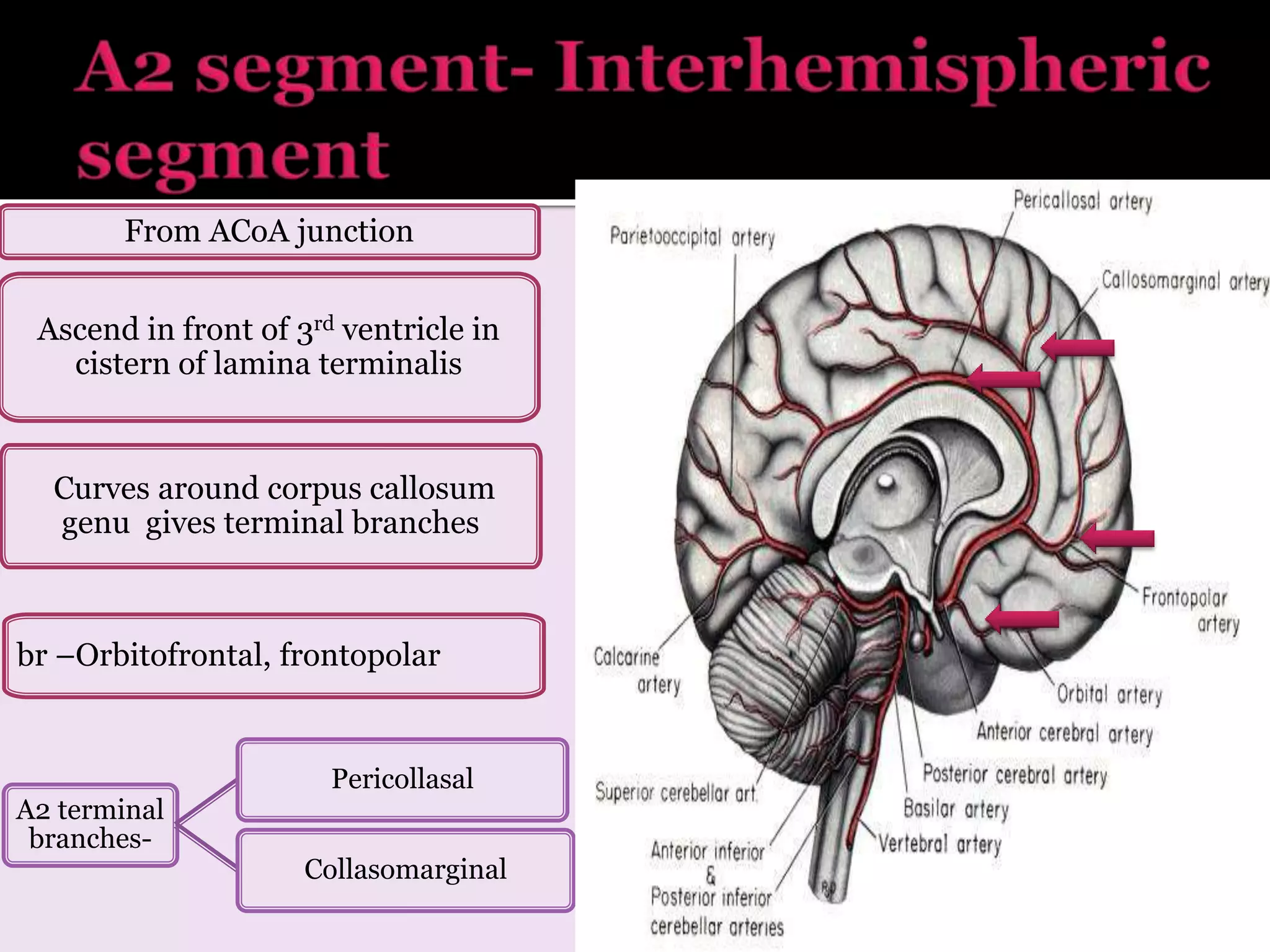
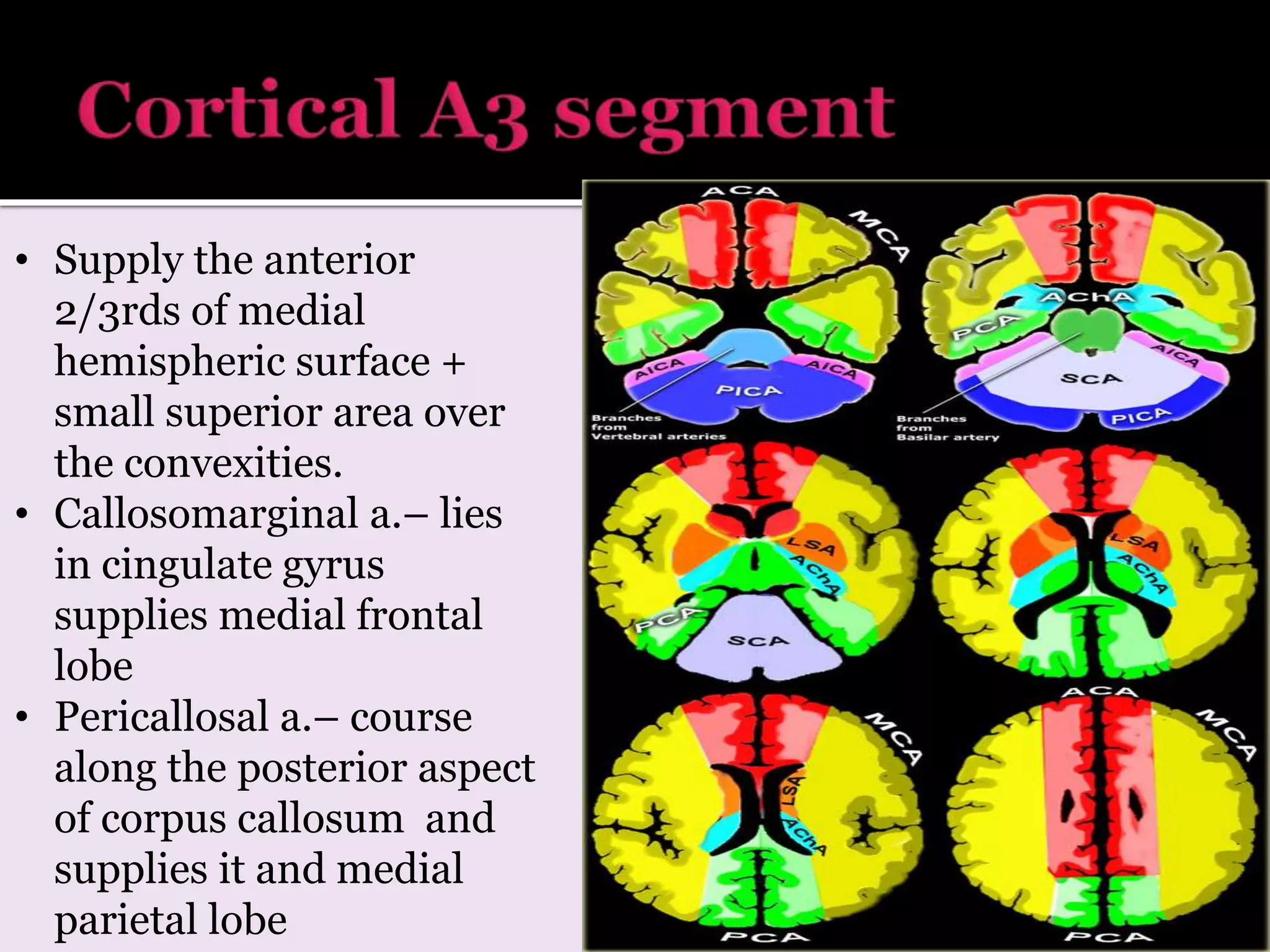
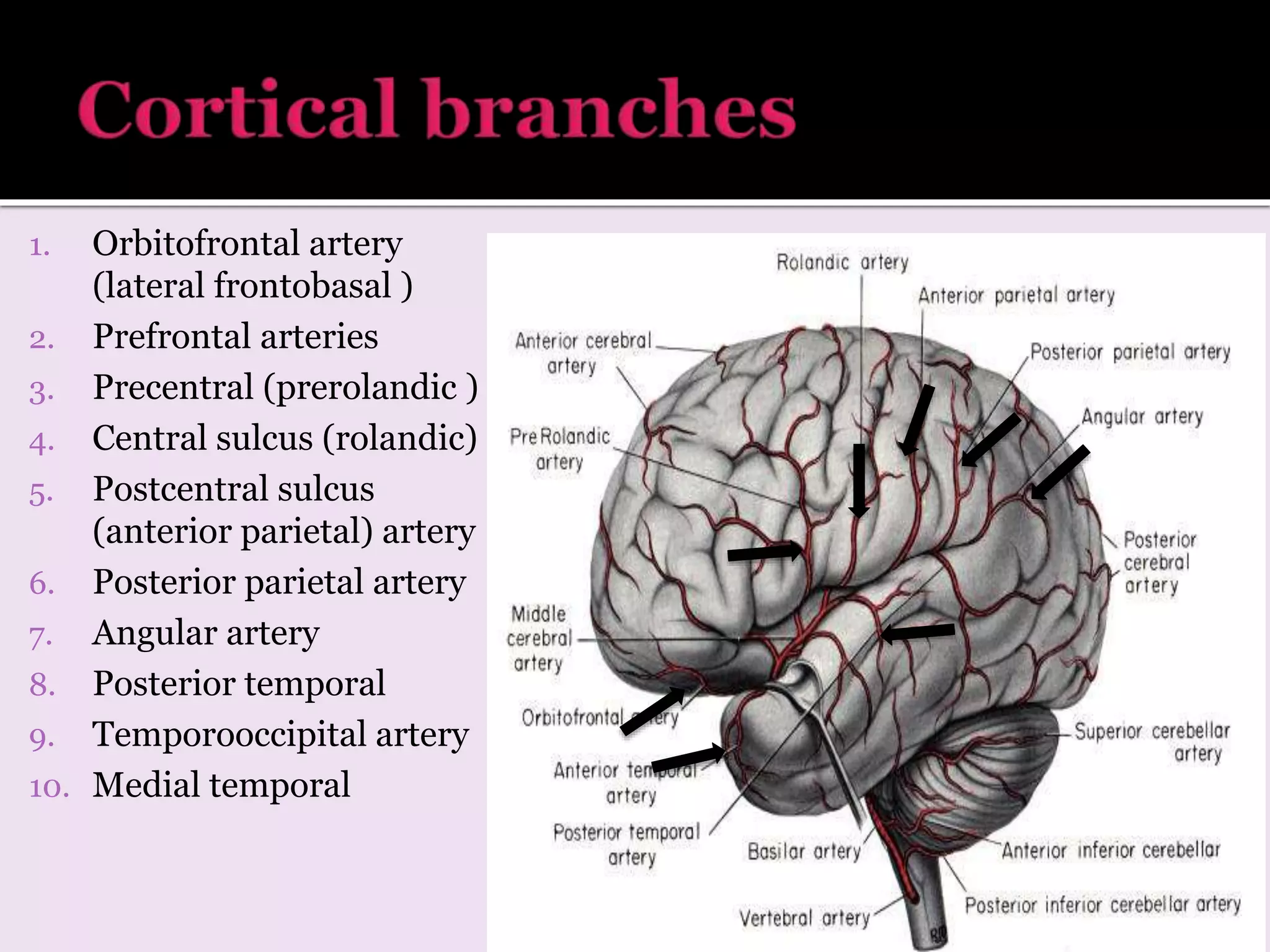
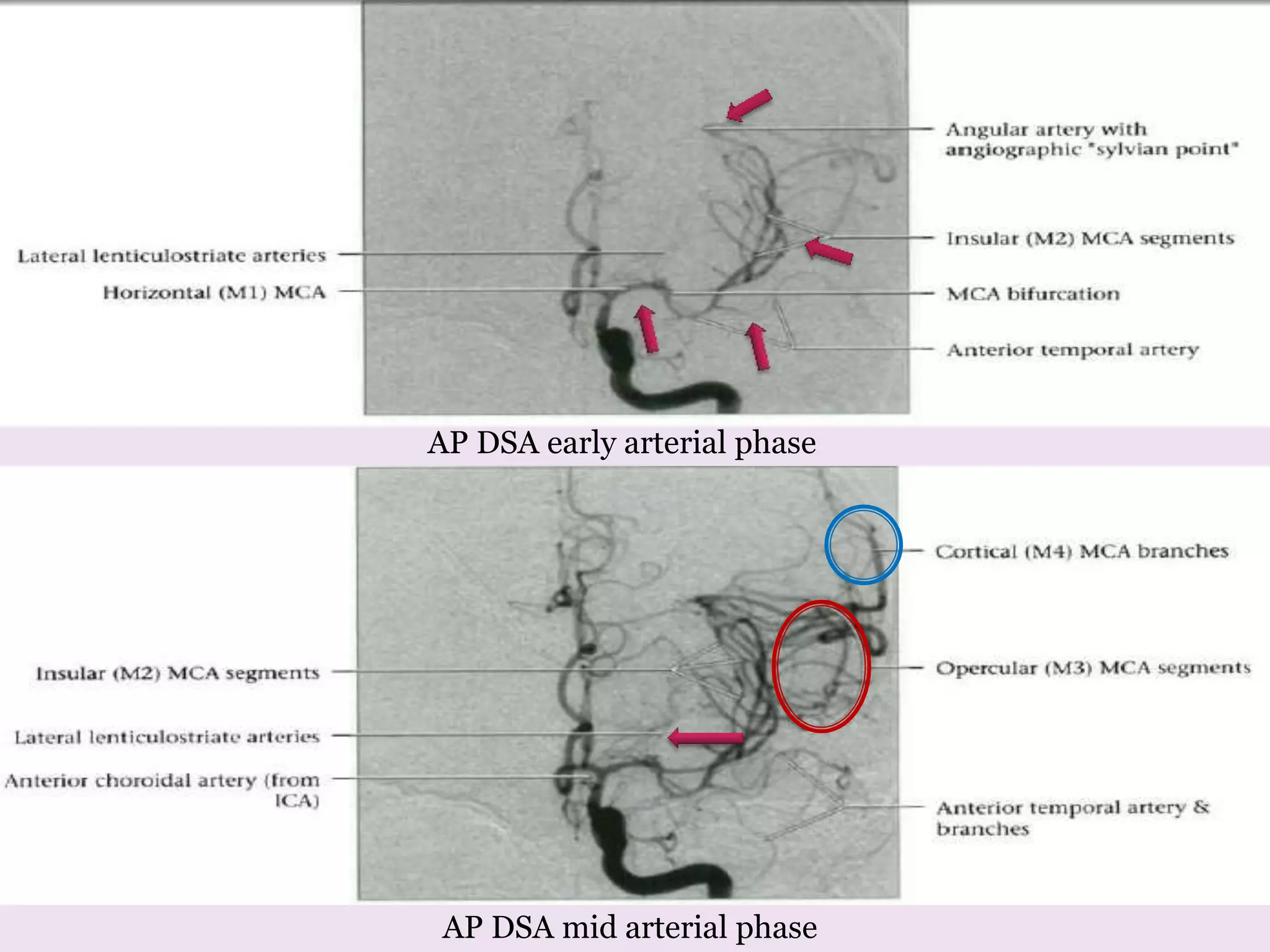
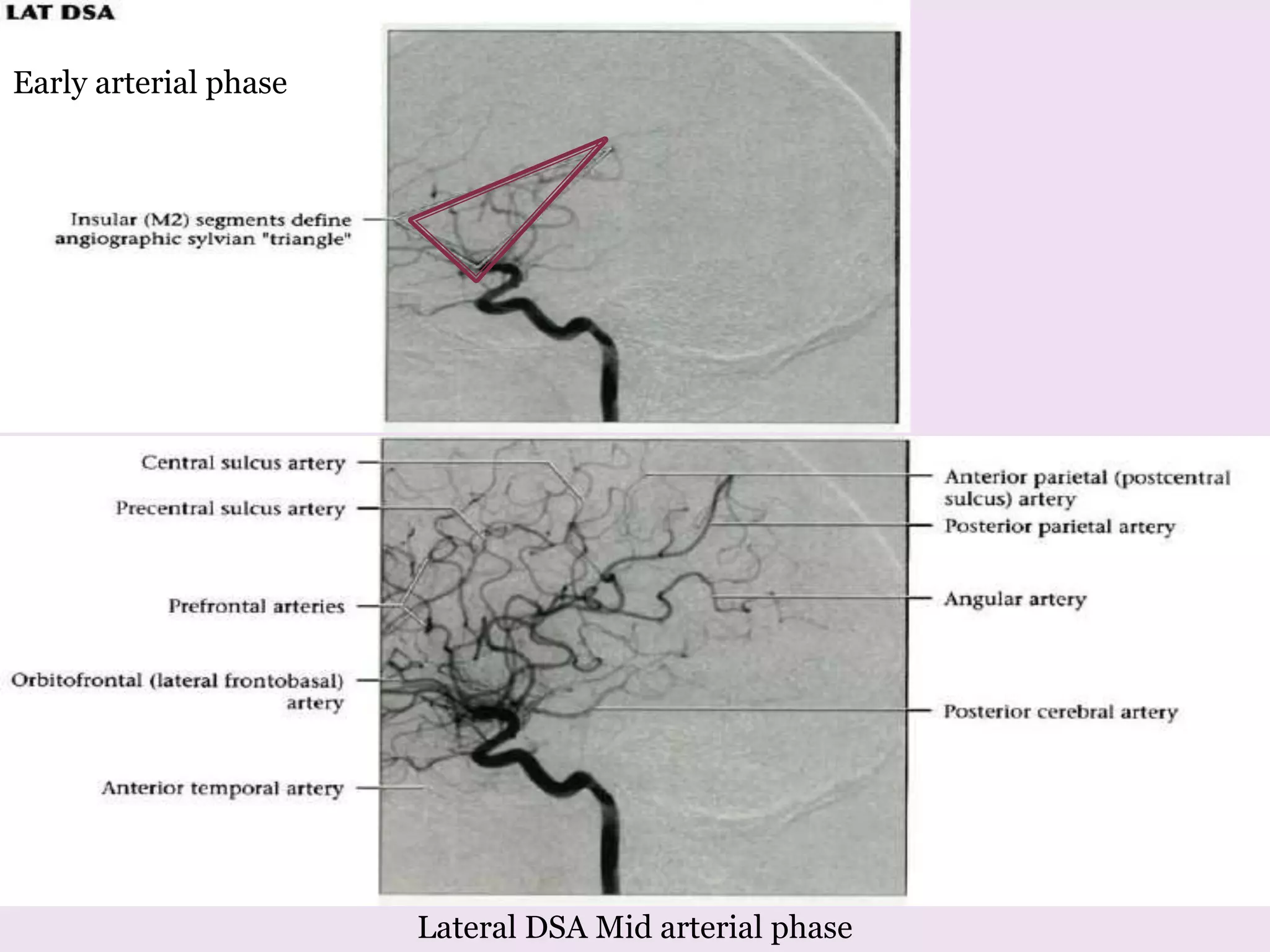
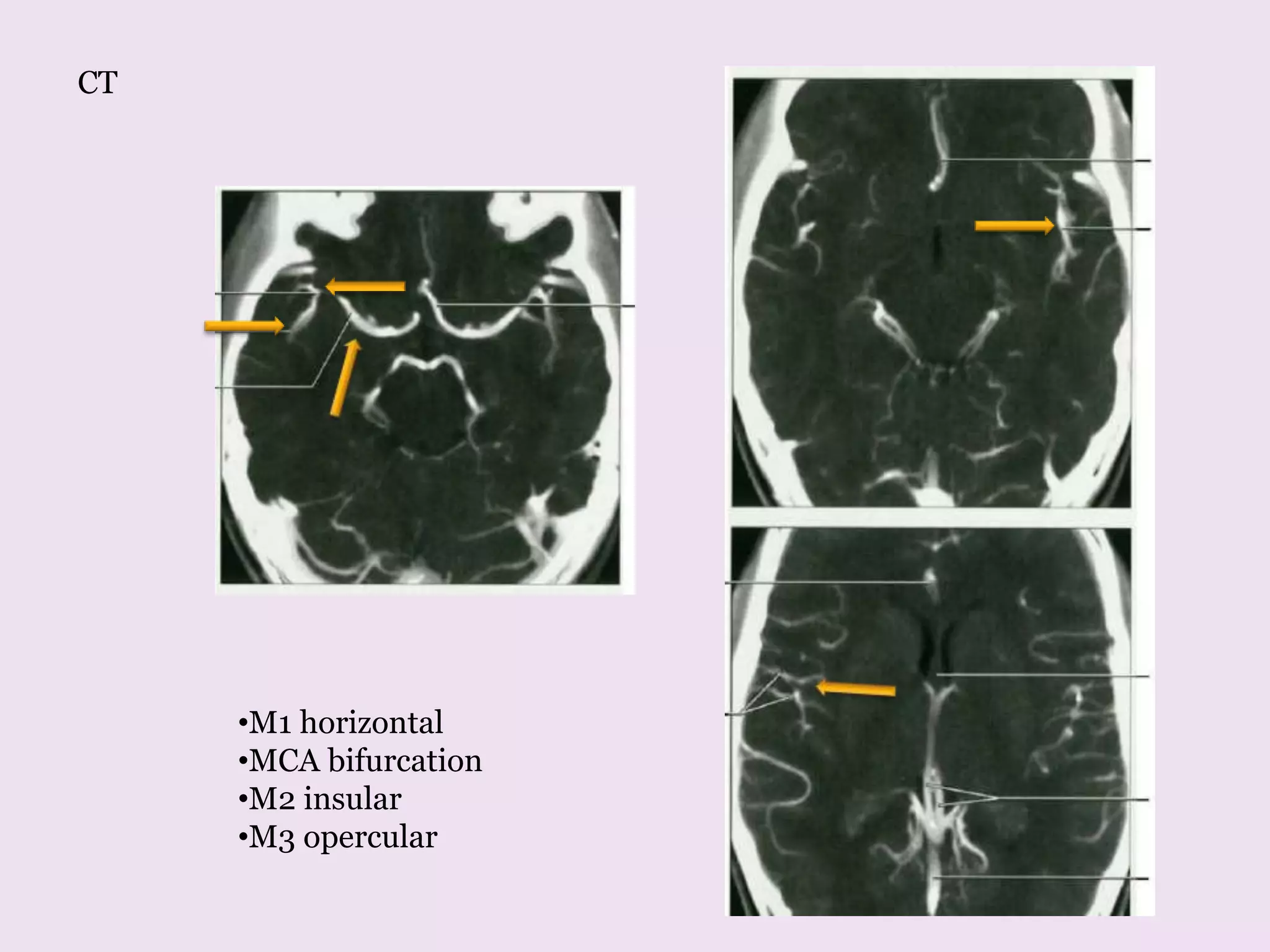
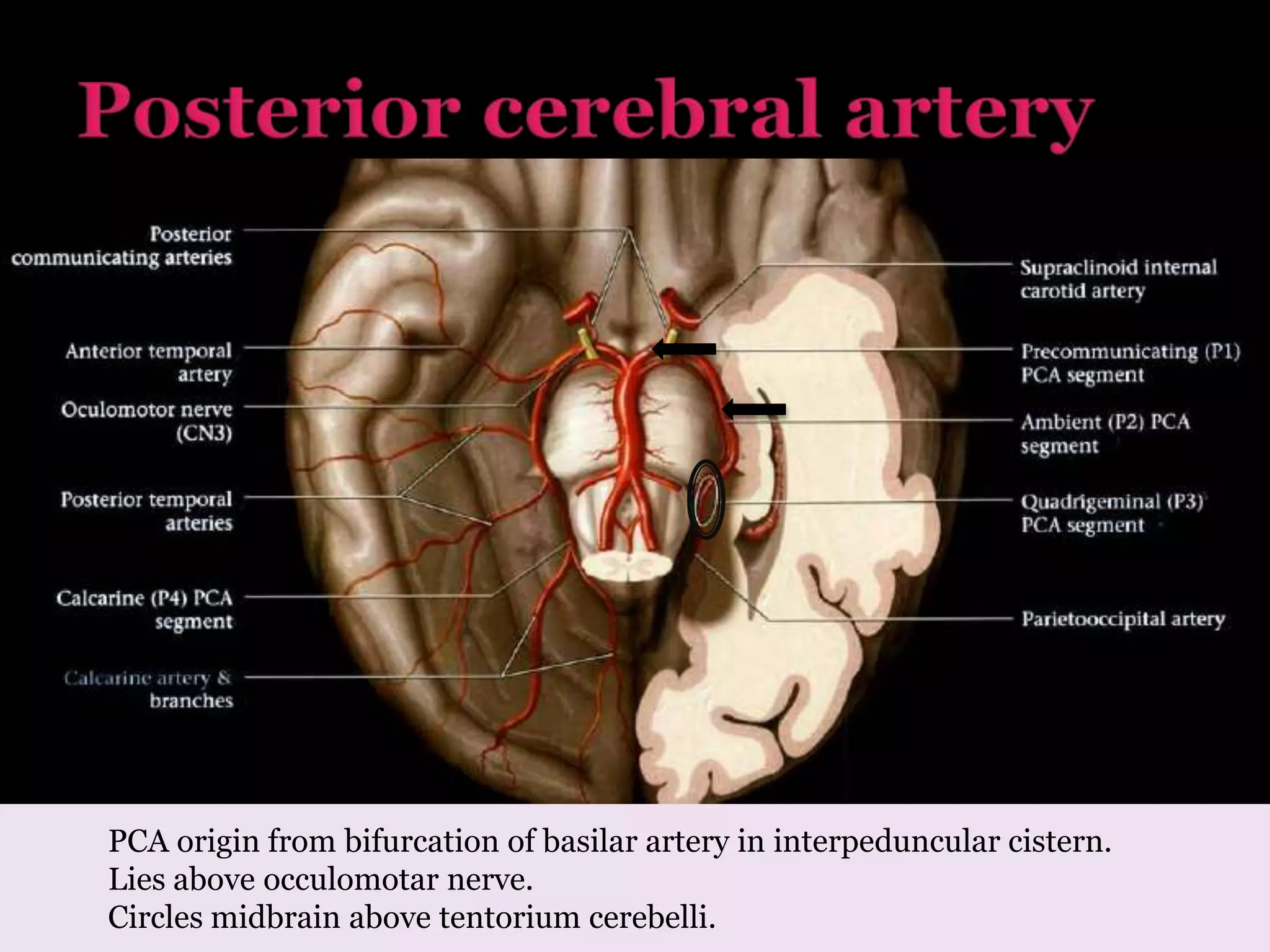
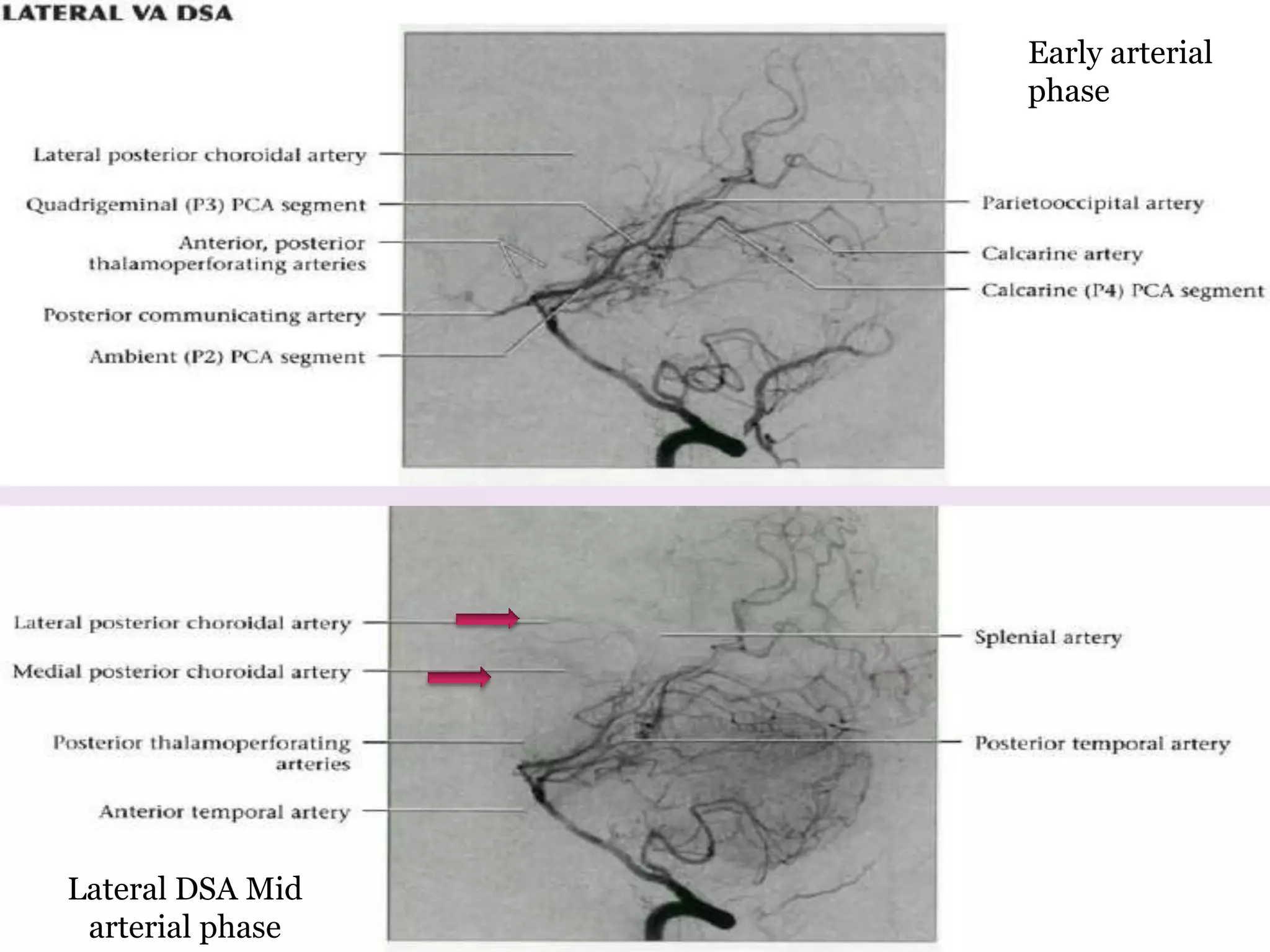
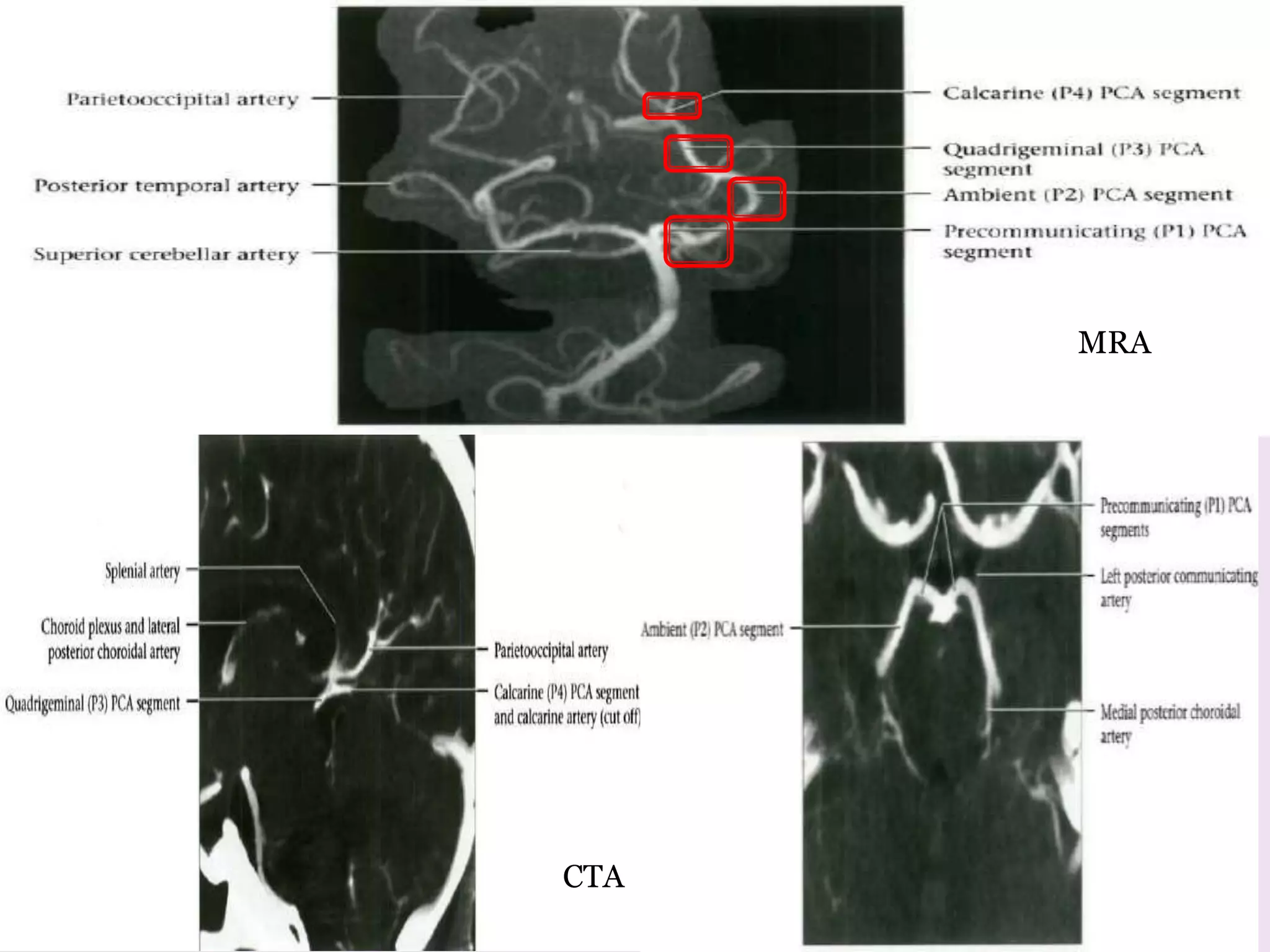
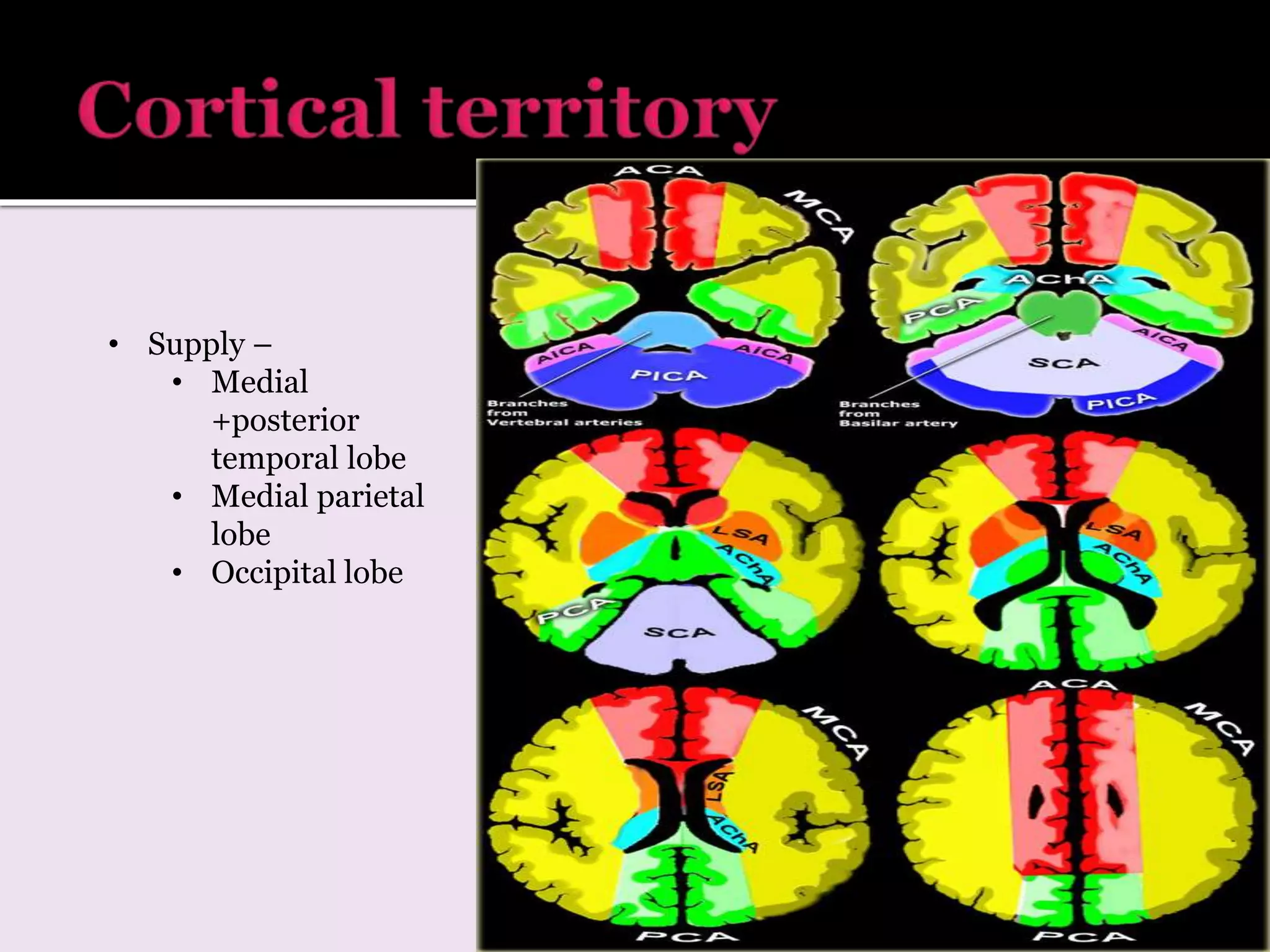
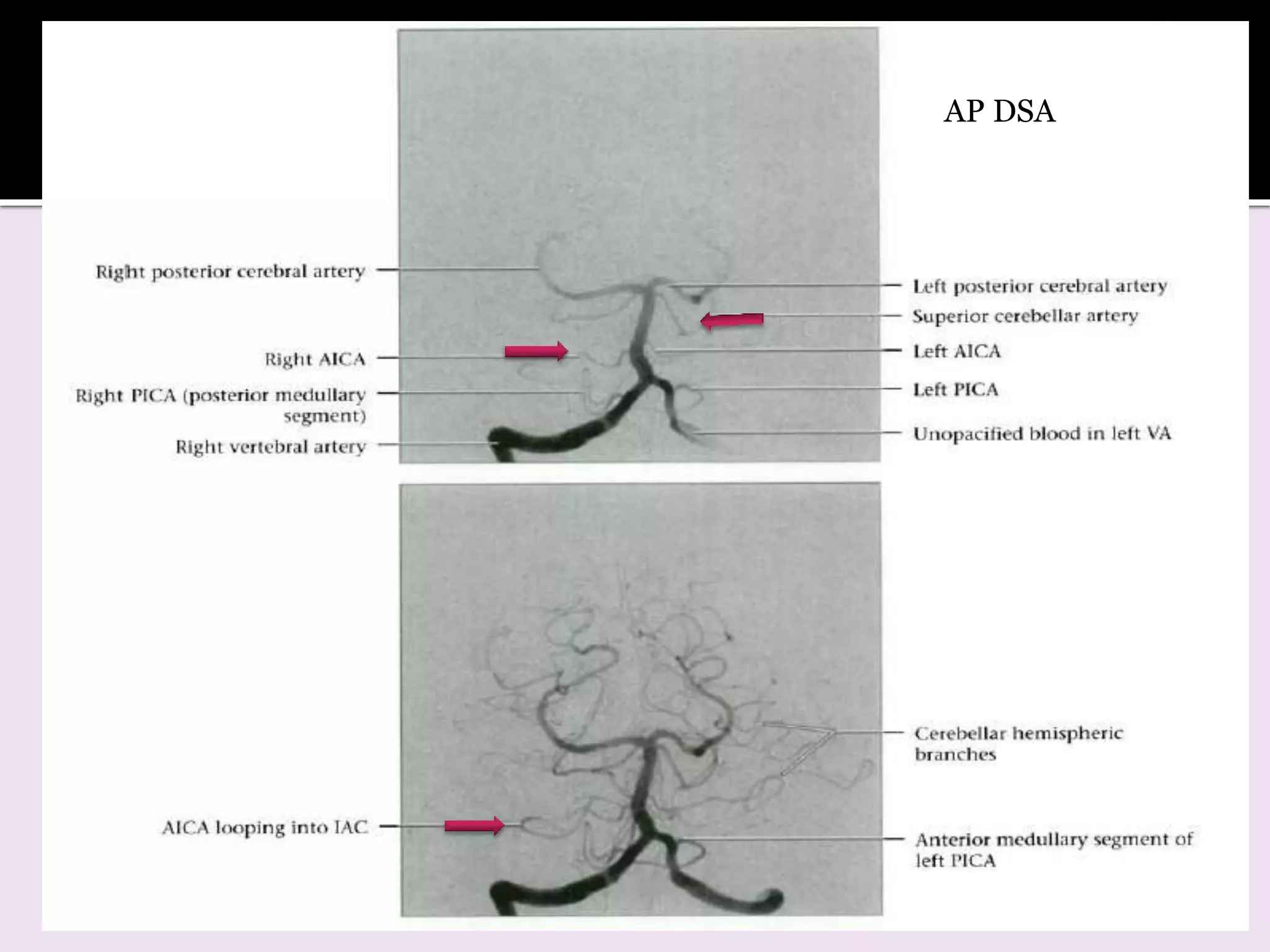
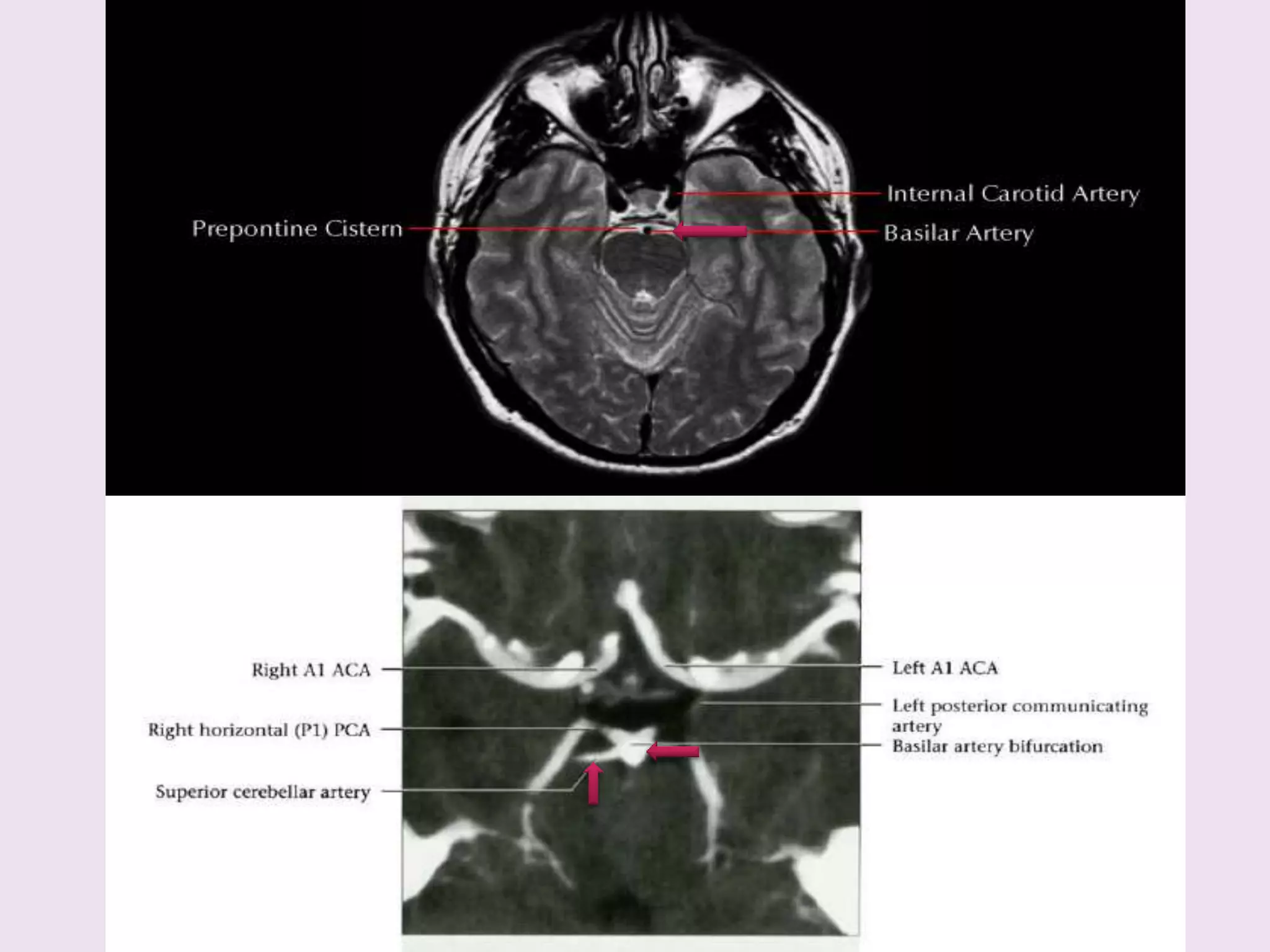
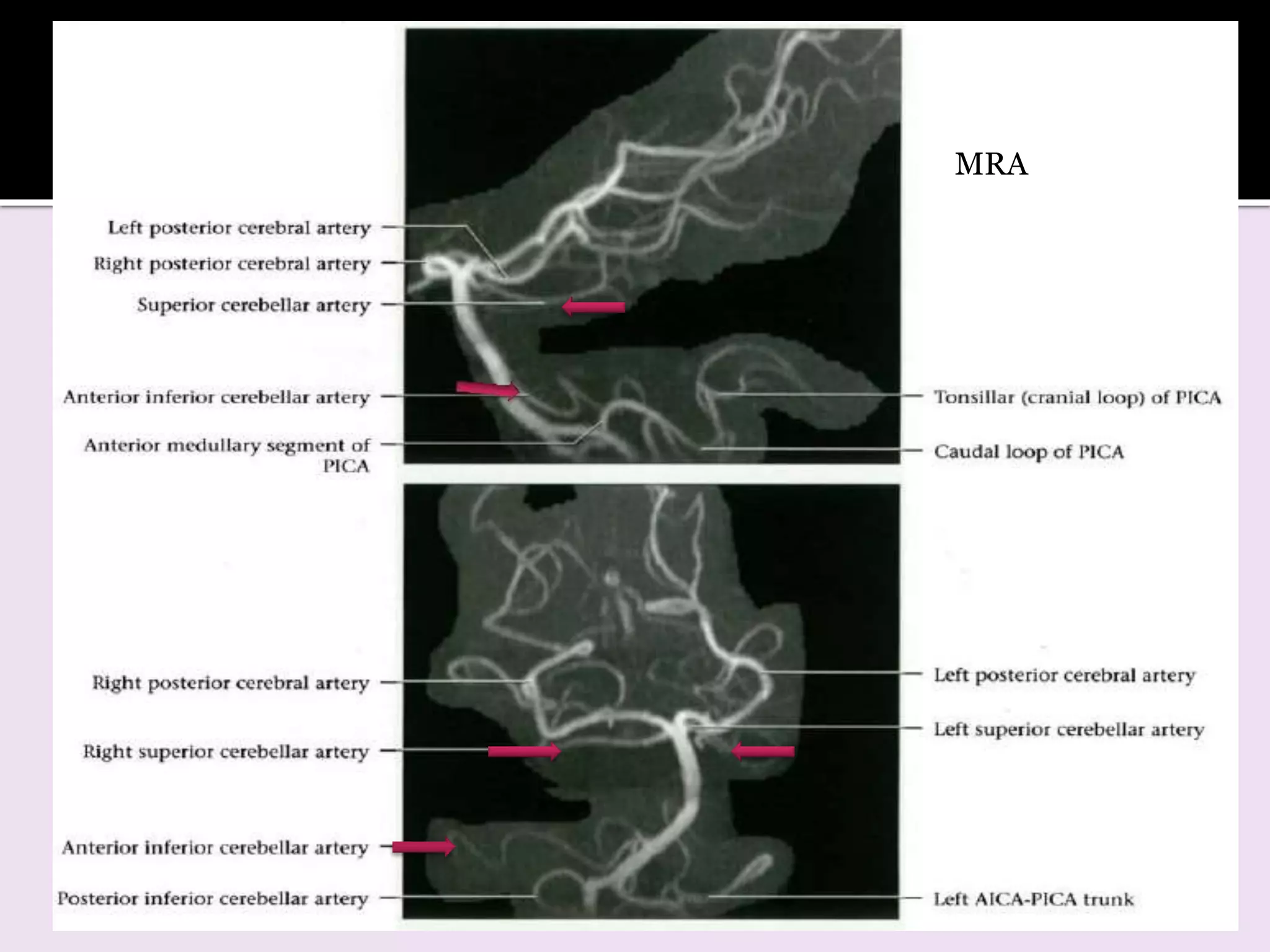
1. The document describes the anatomy and branches of the major cerebral arteries including the anterior, middle, and posterior cerebral arteries.
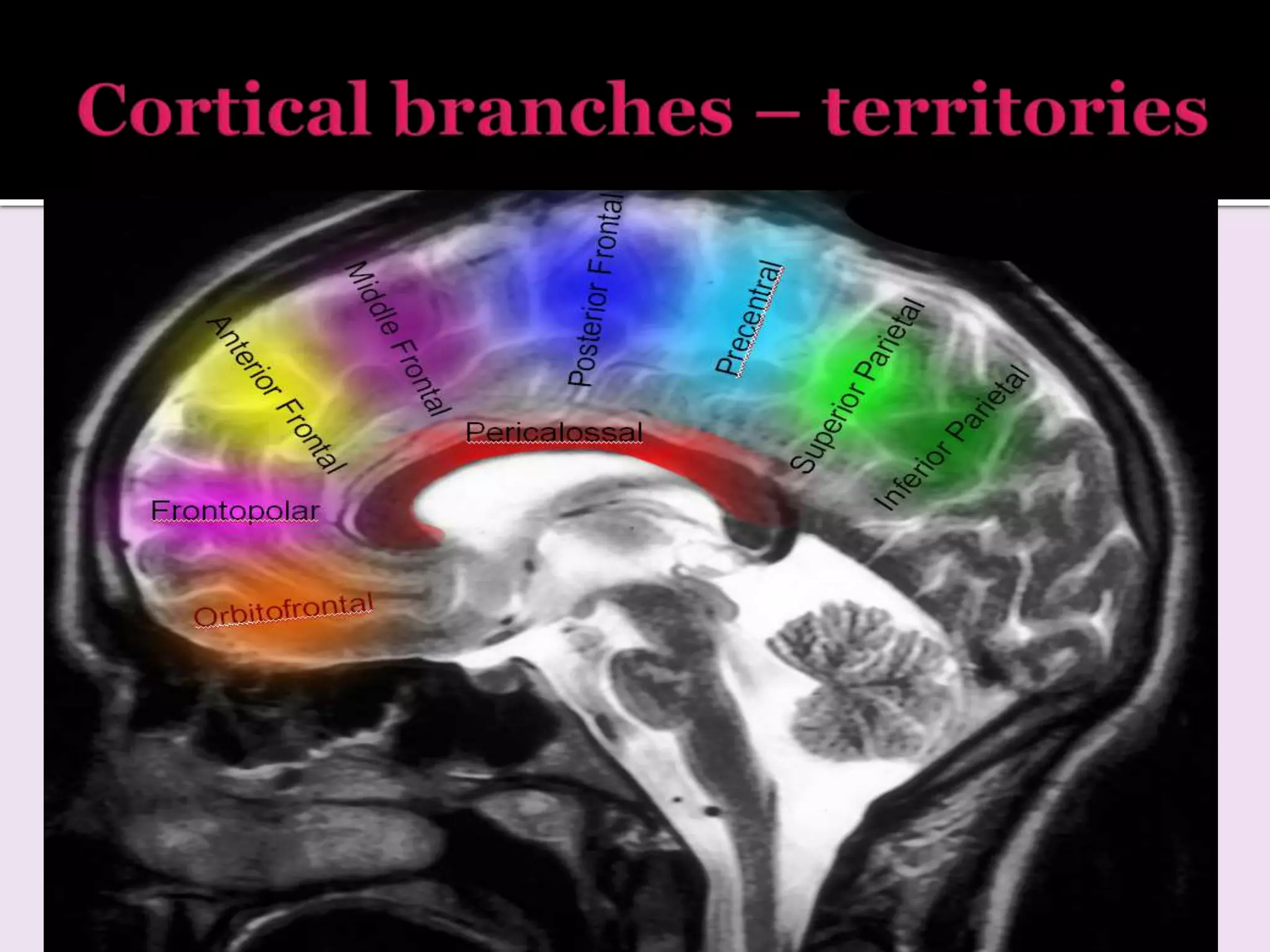
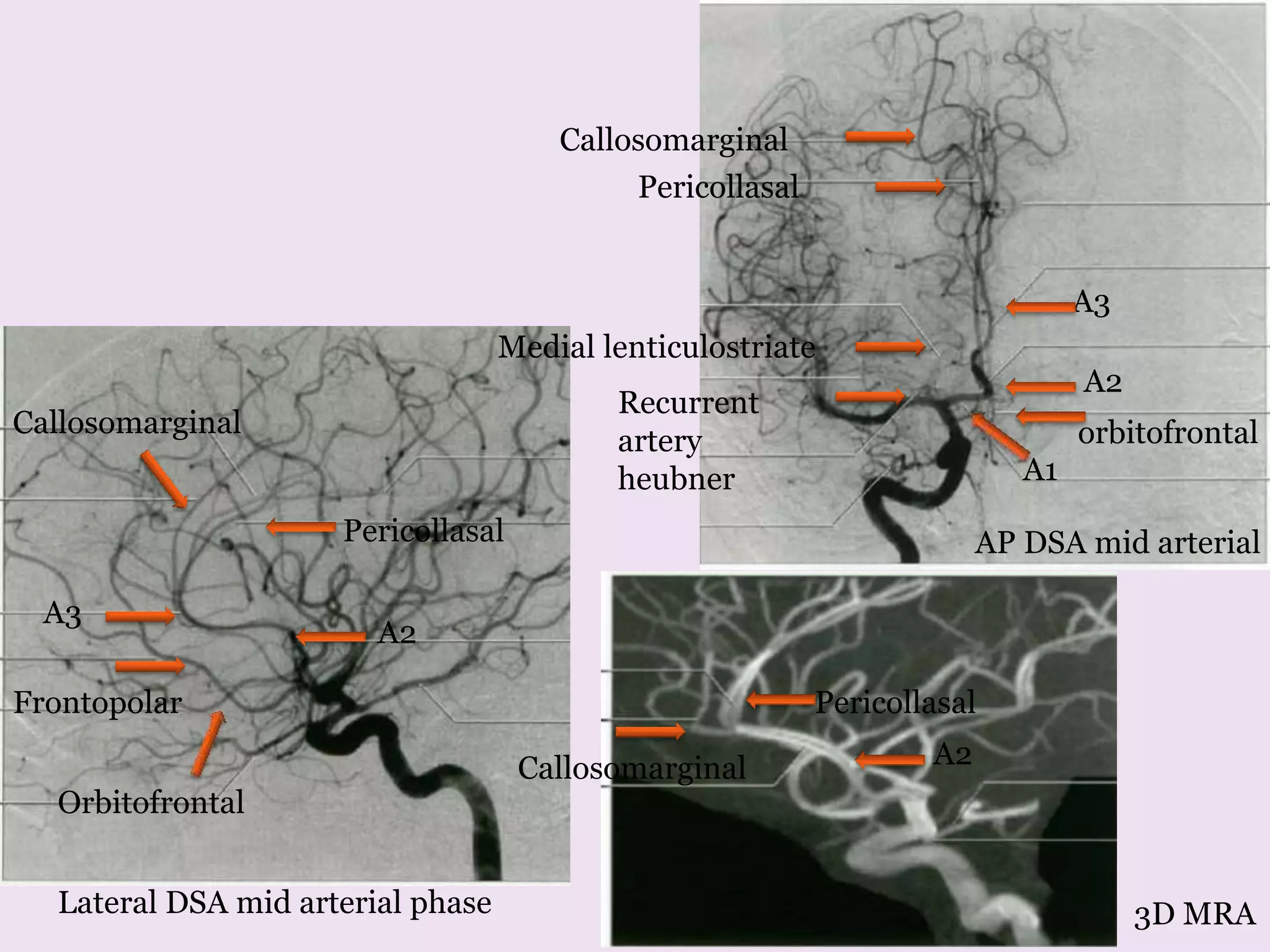
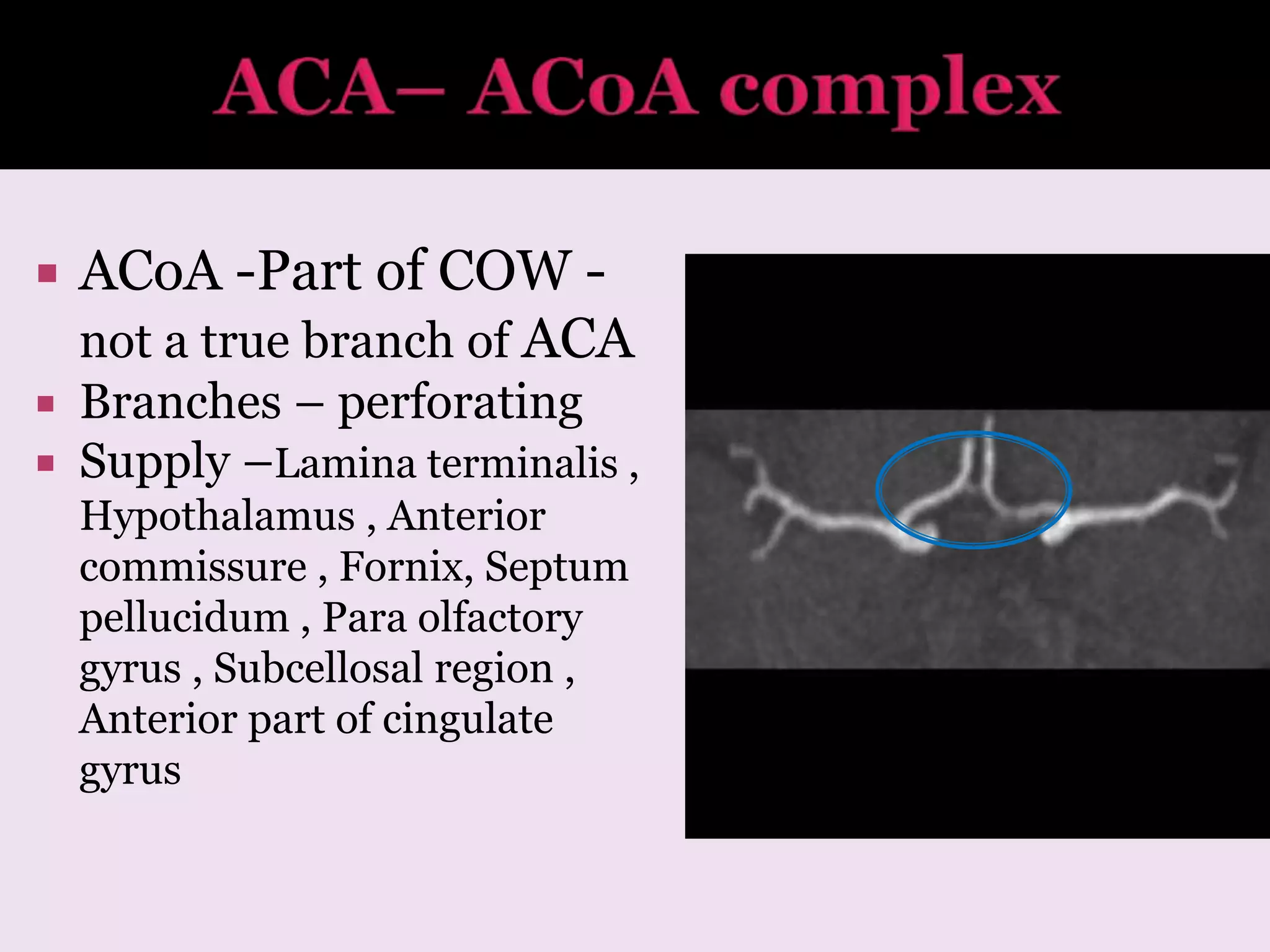
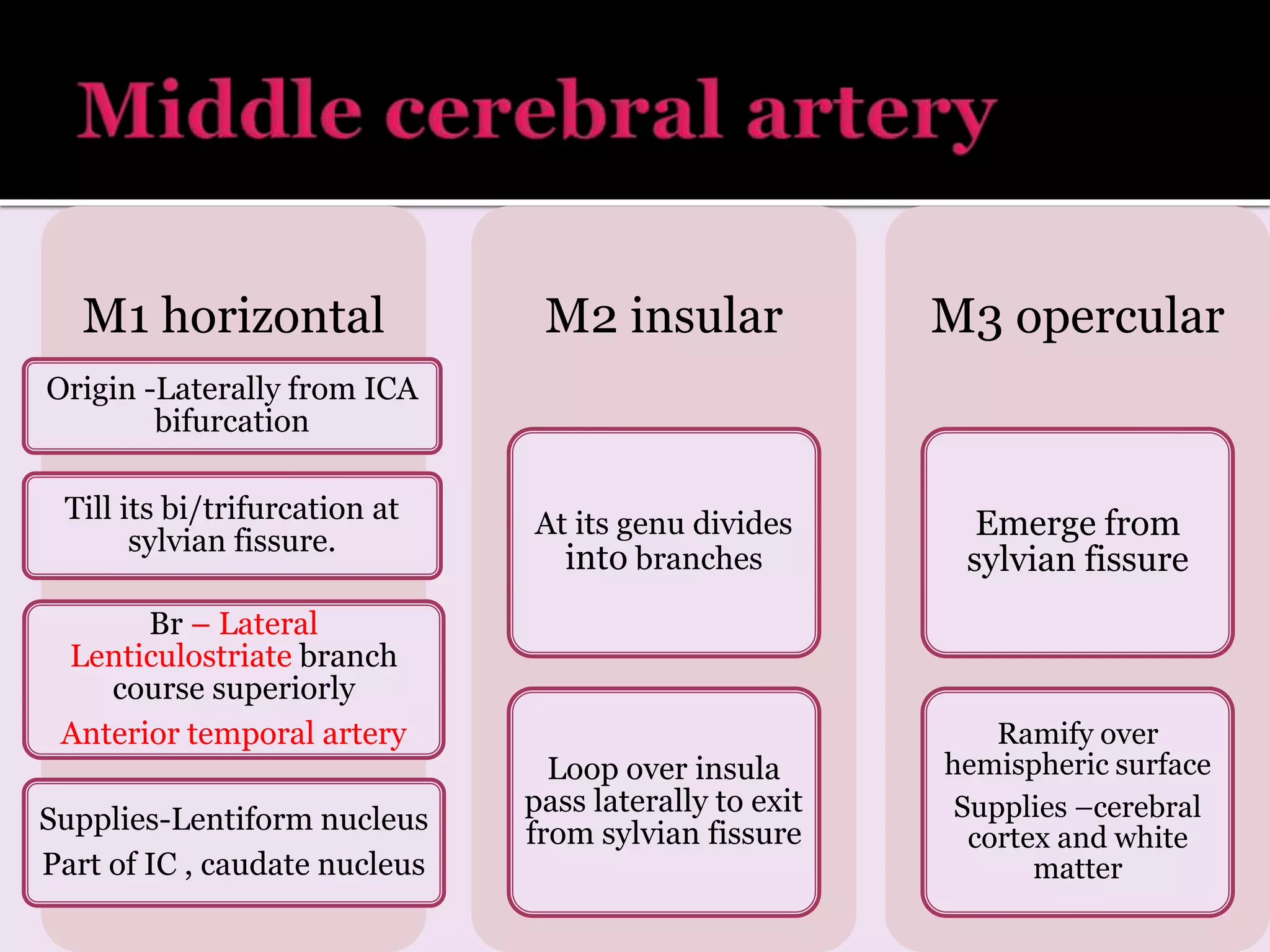
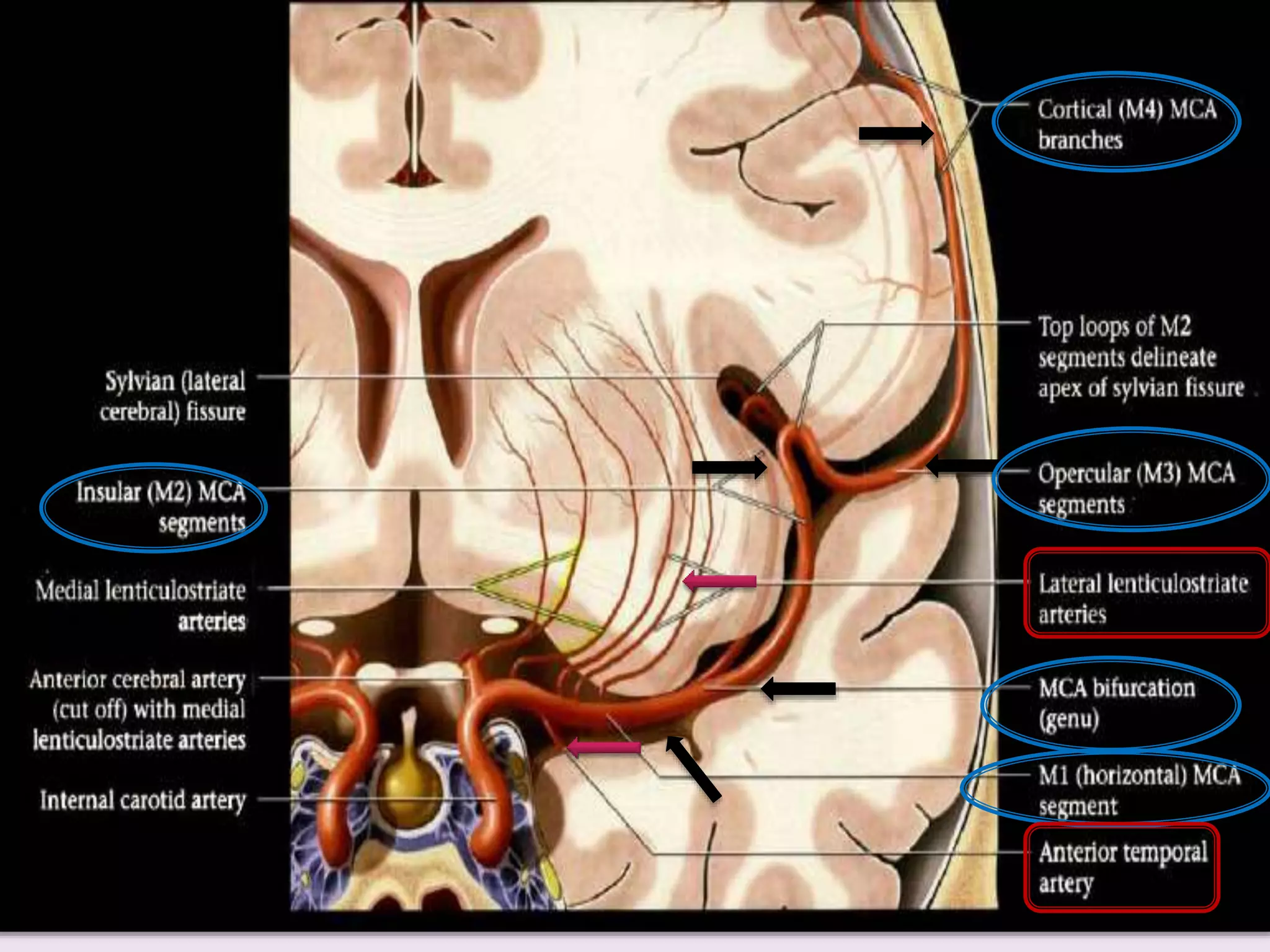
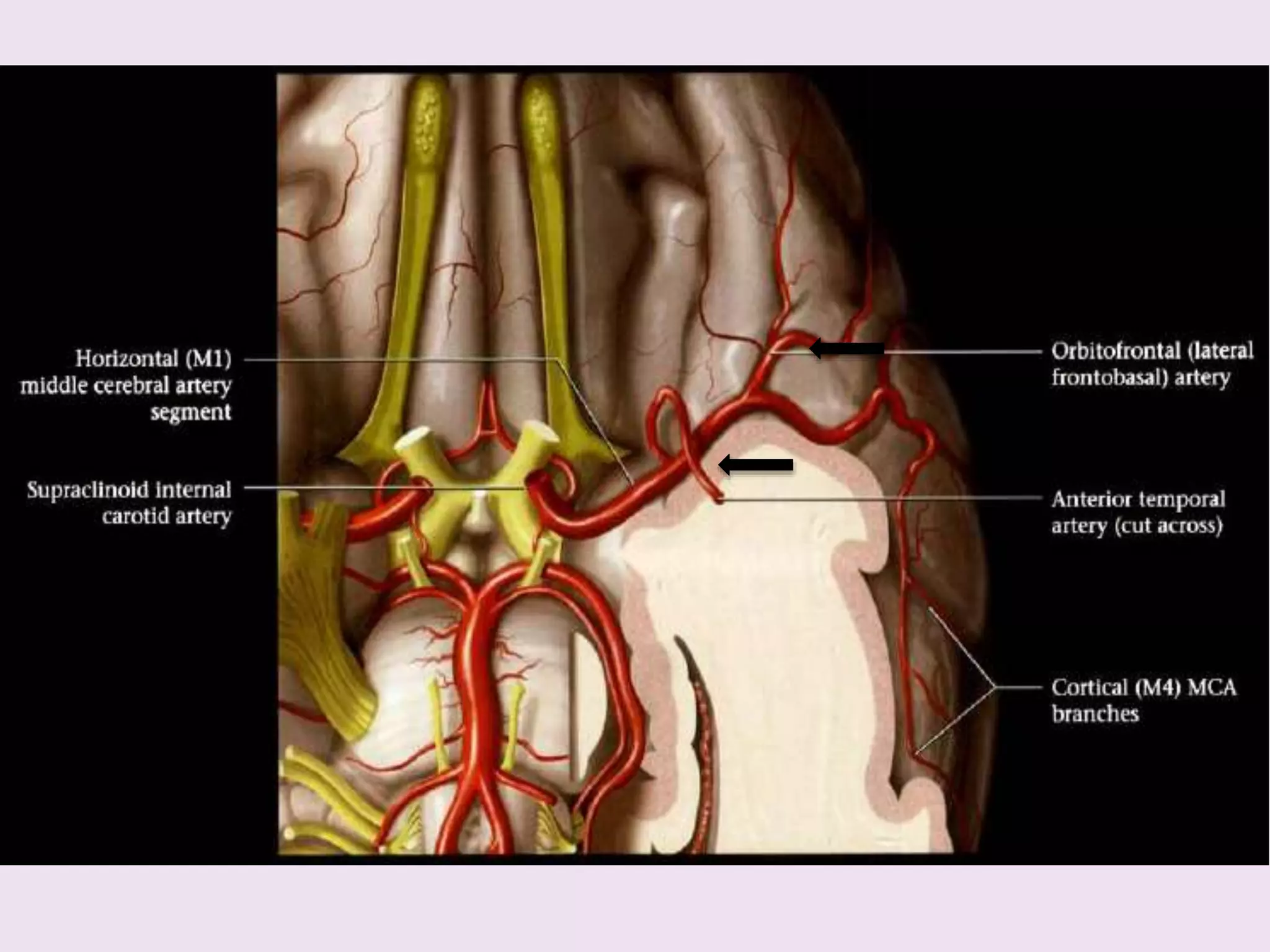
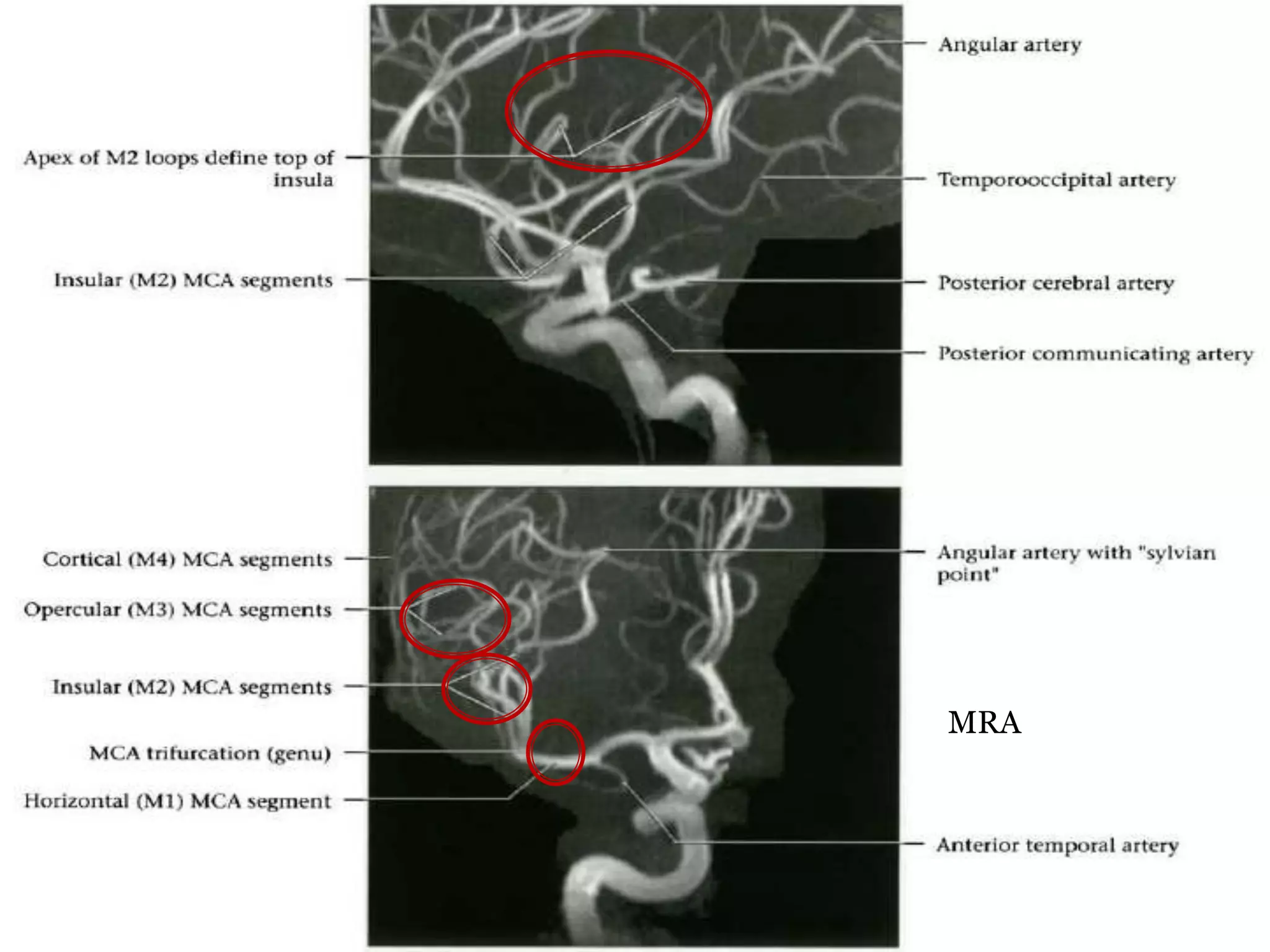
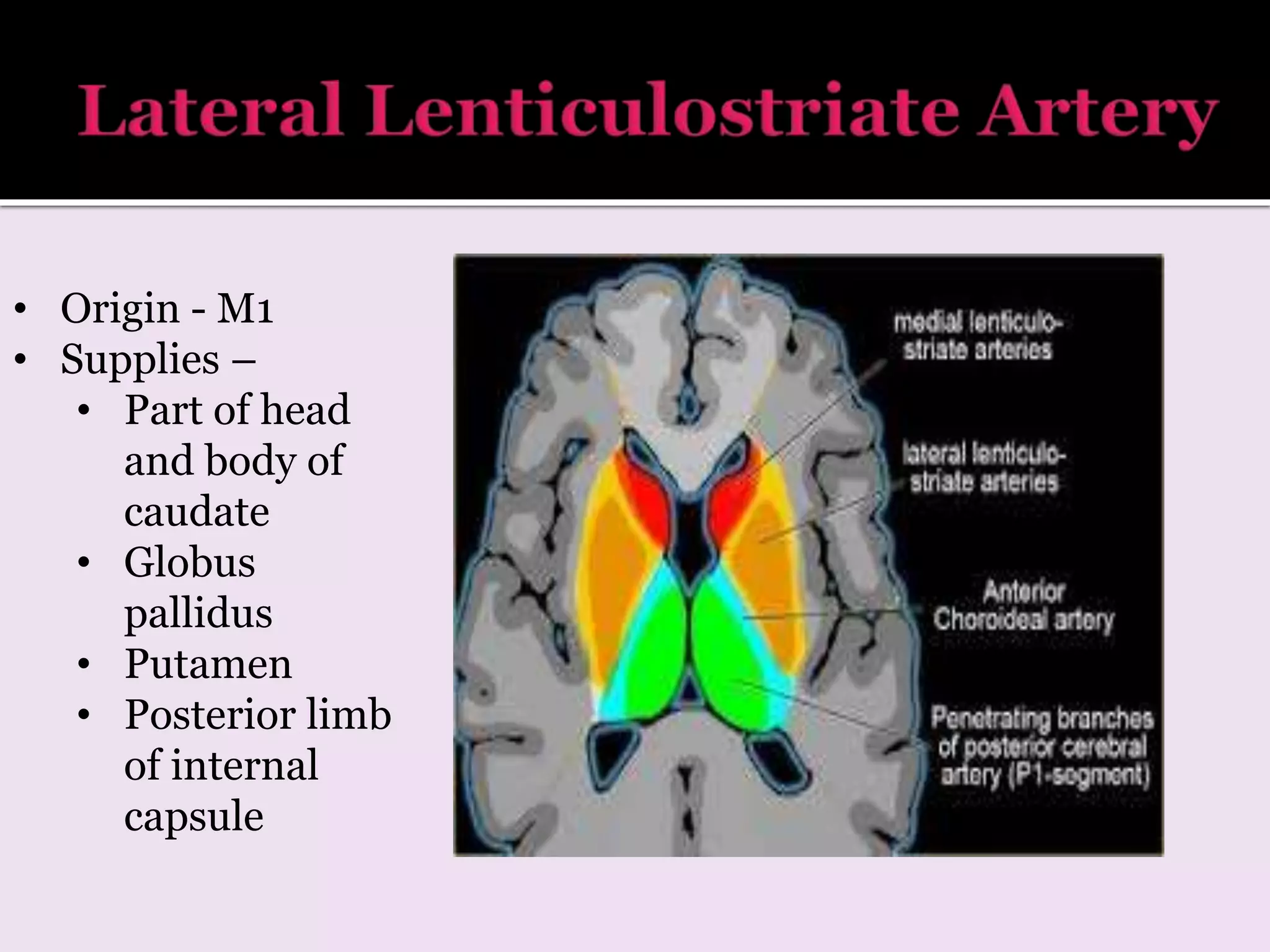
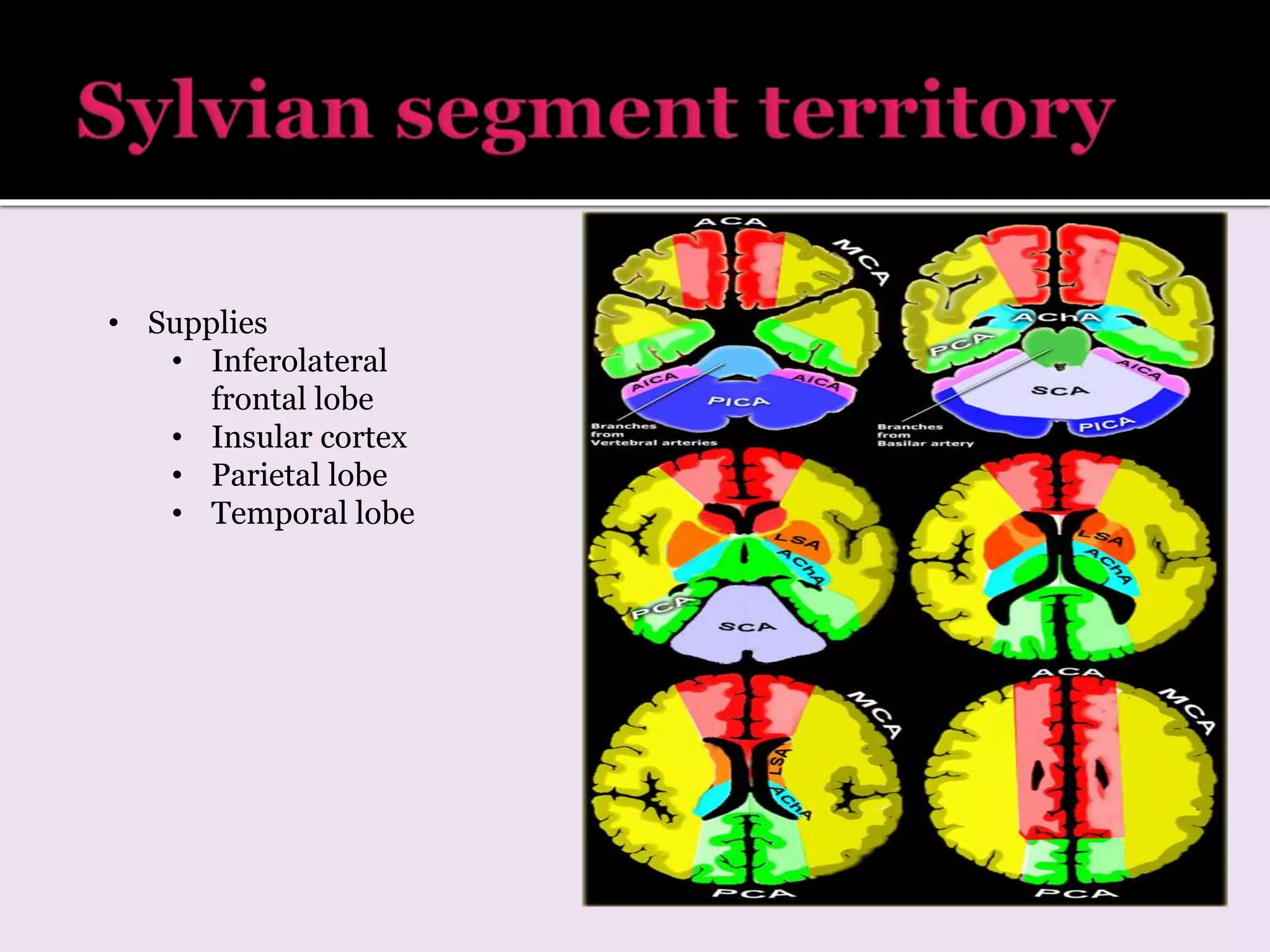
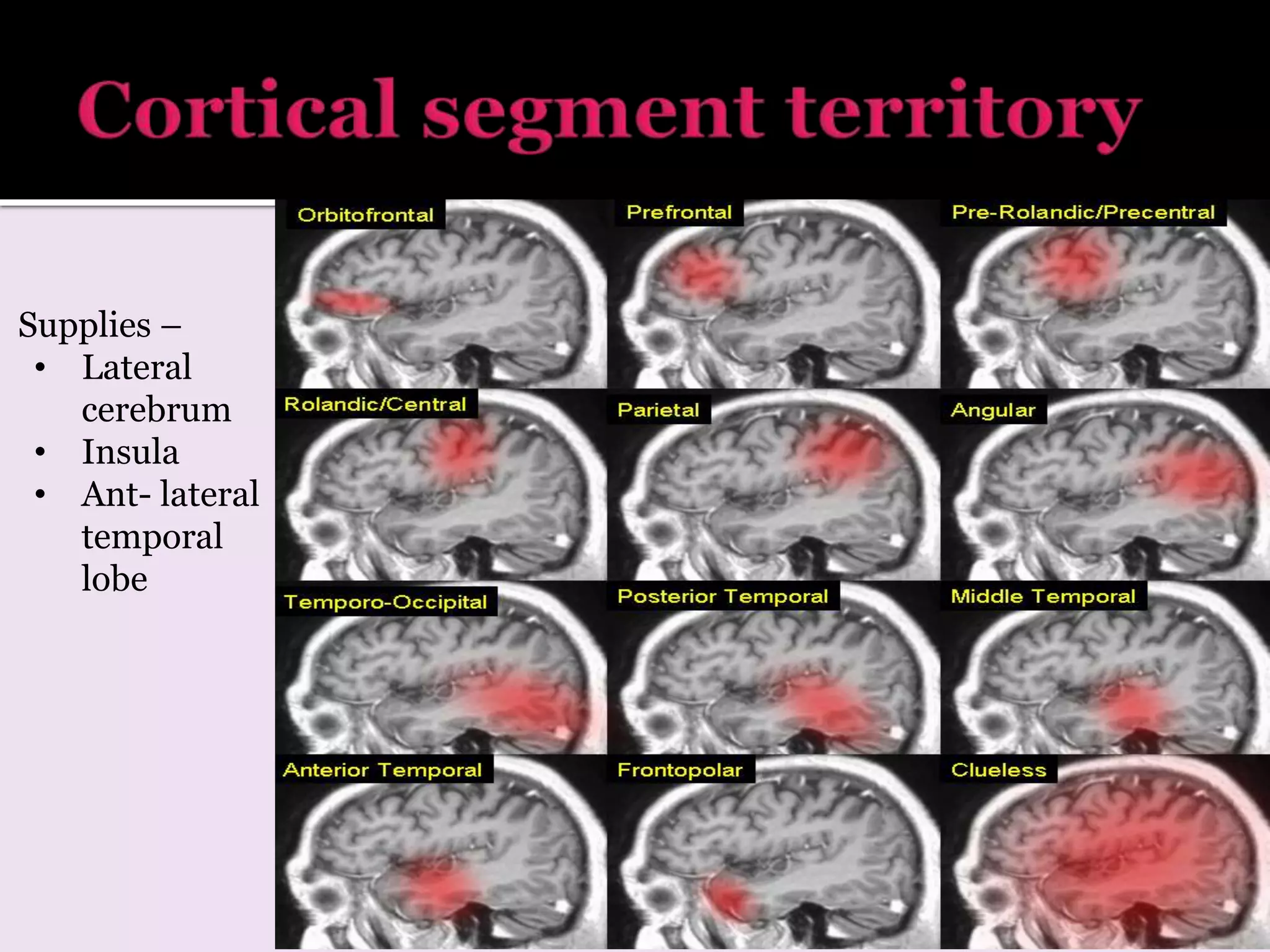
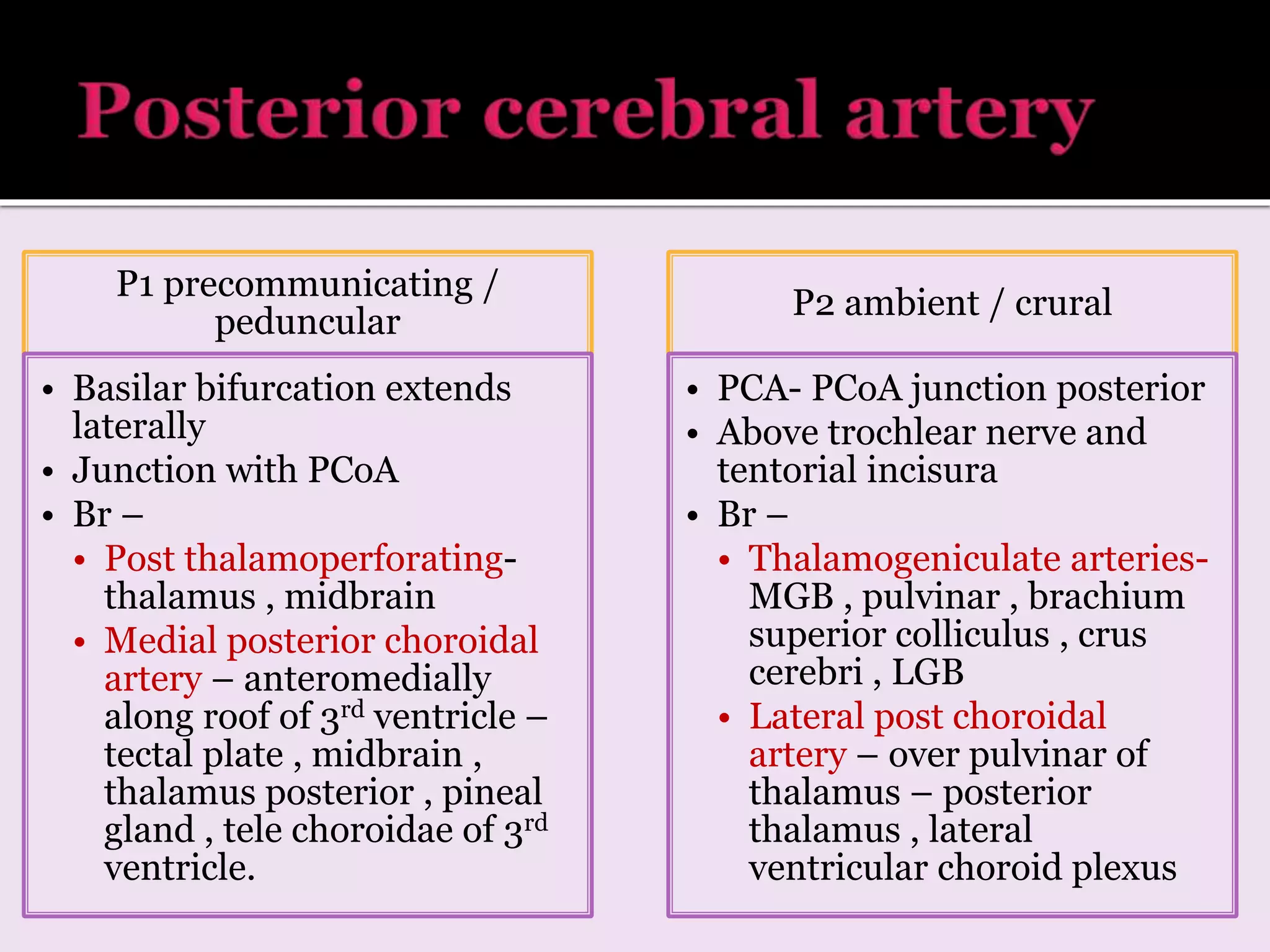
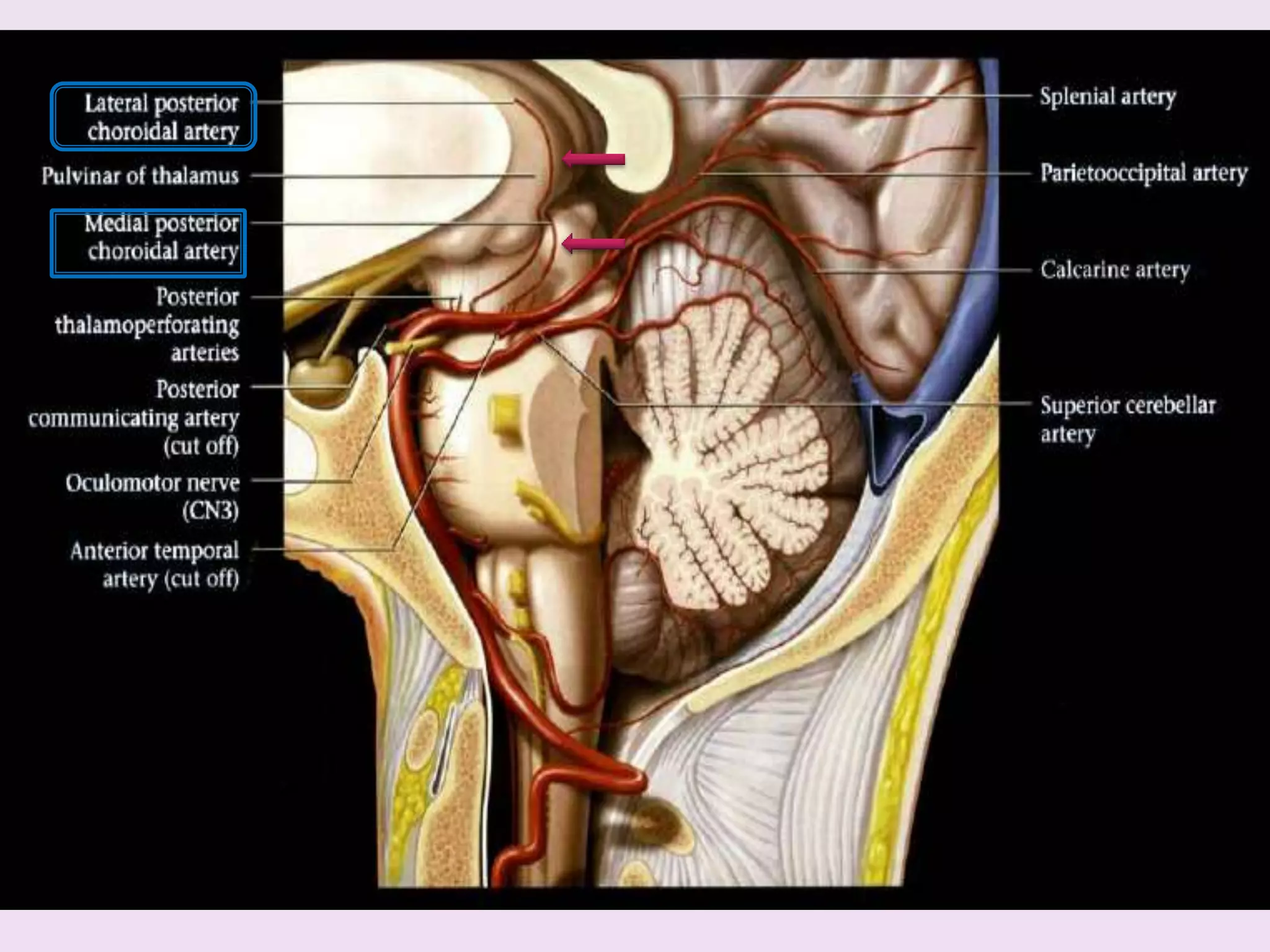
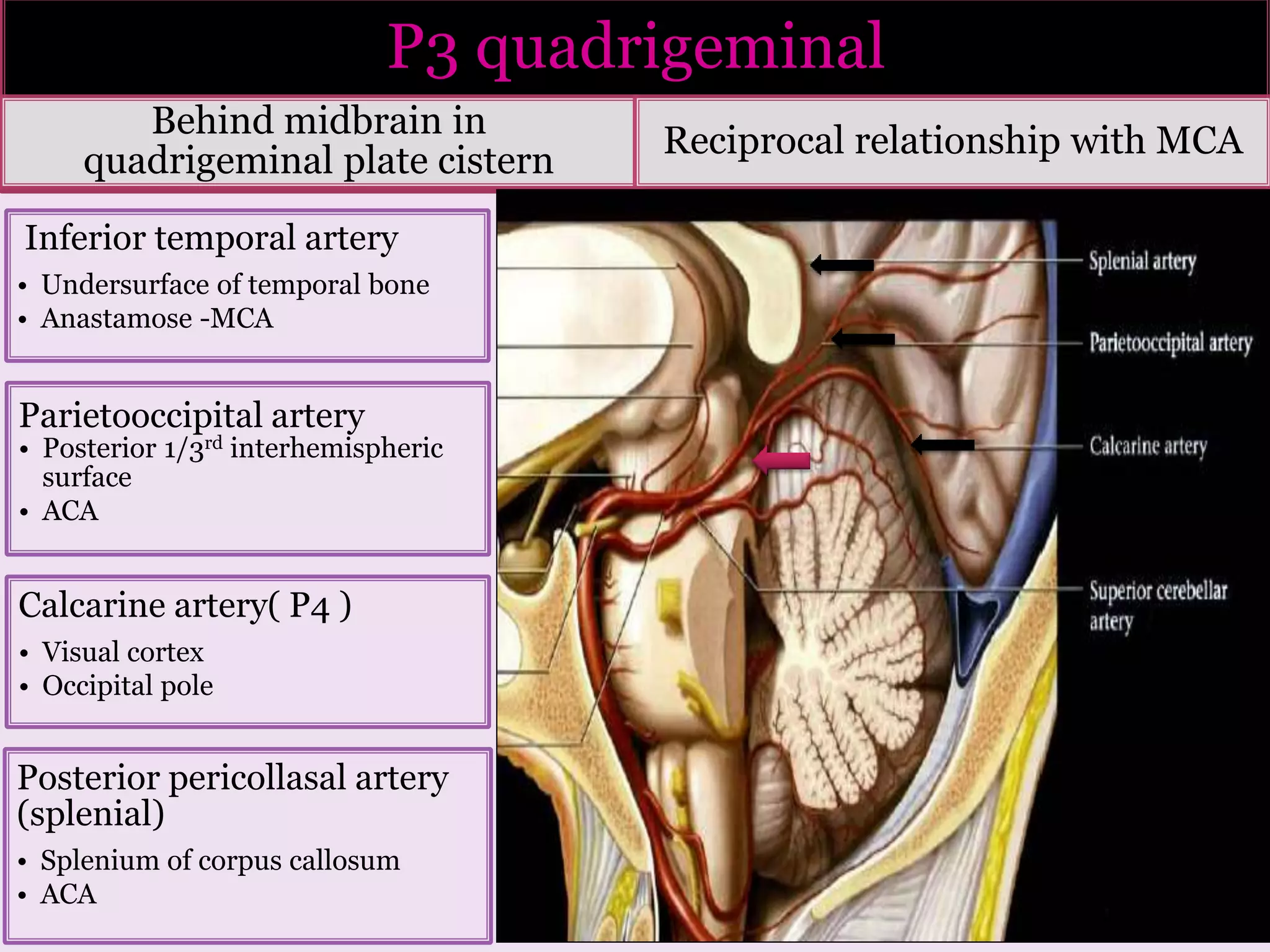
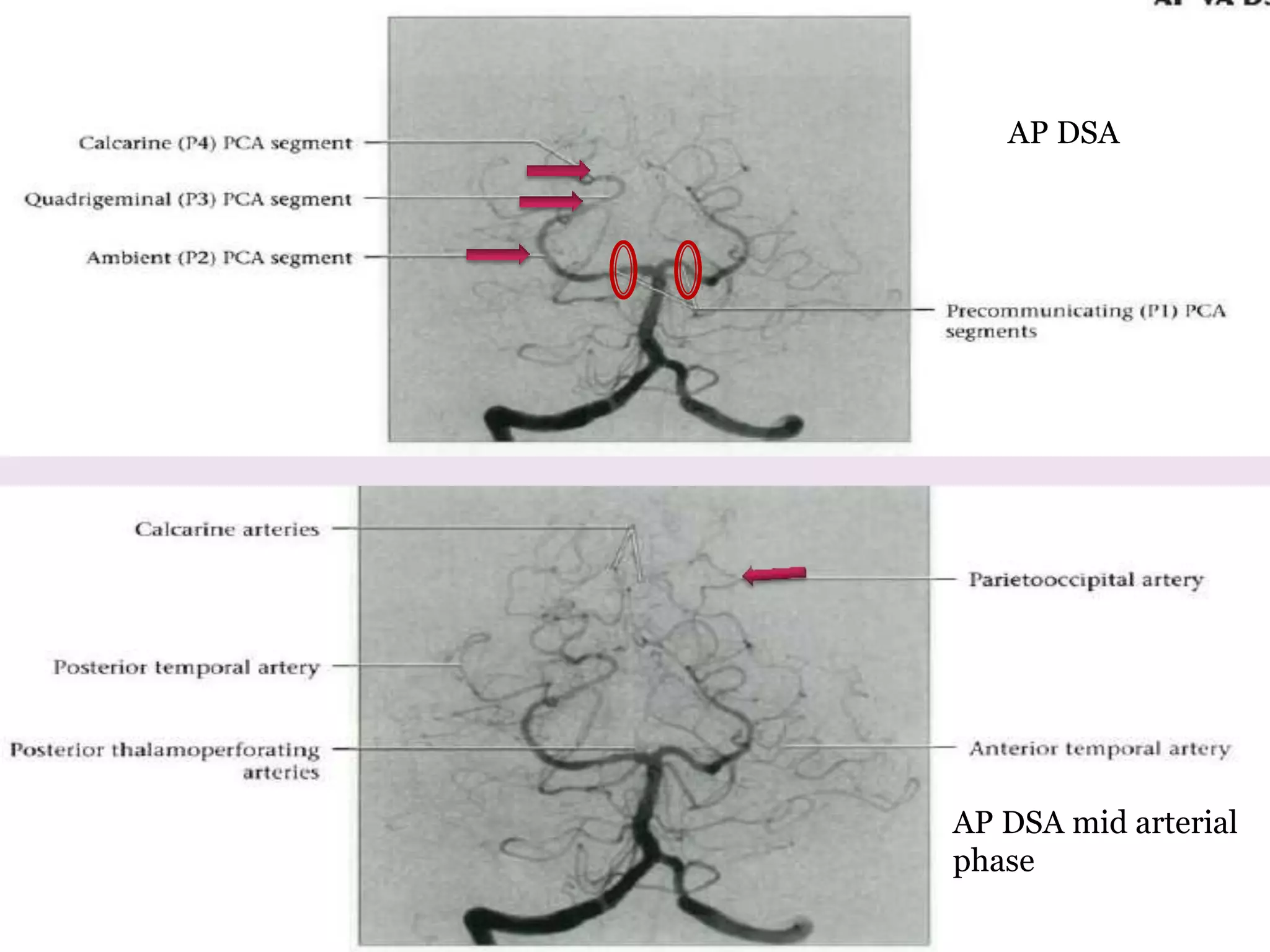
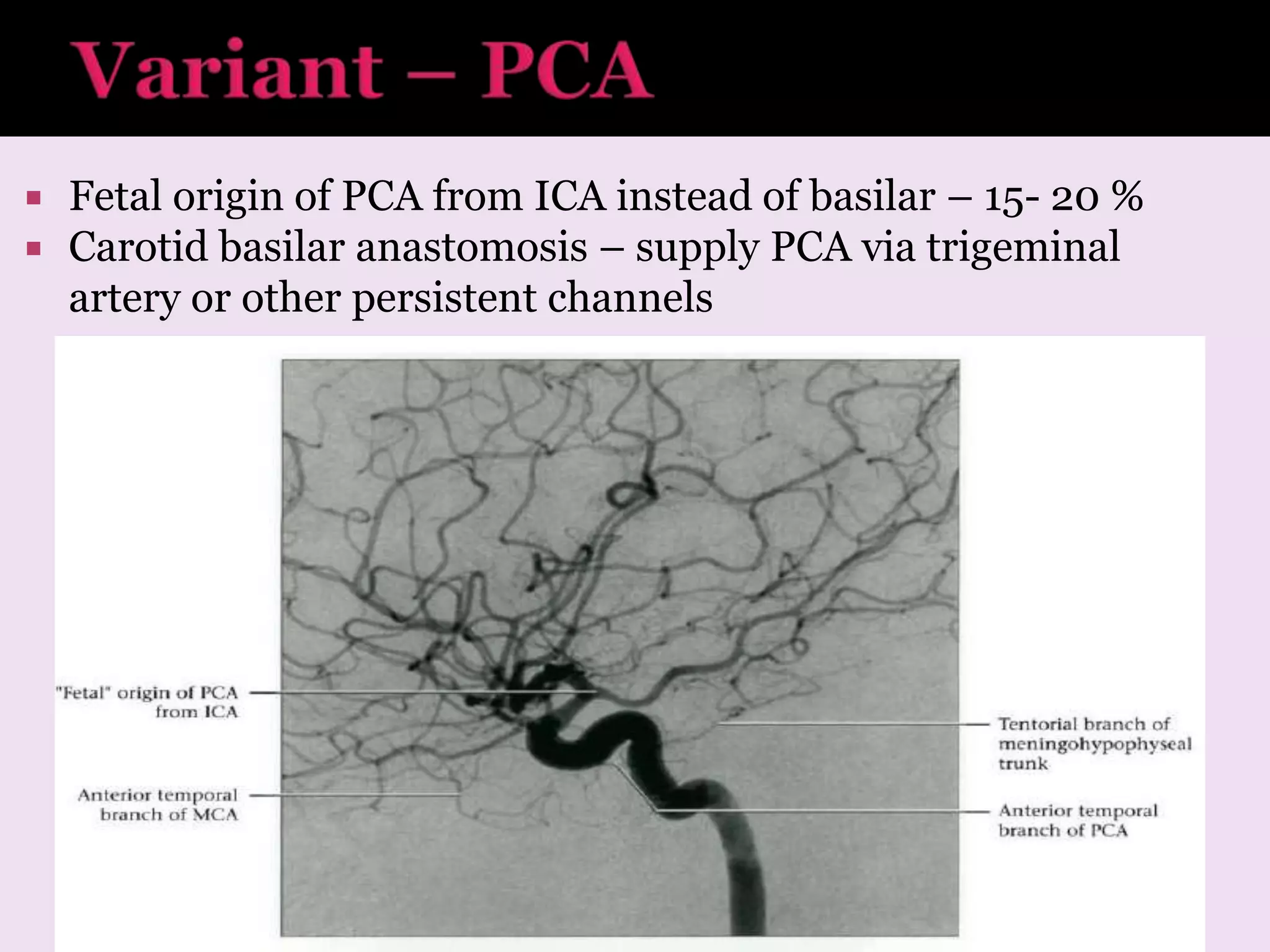
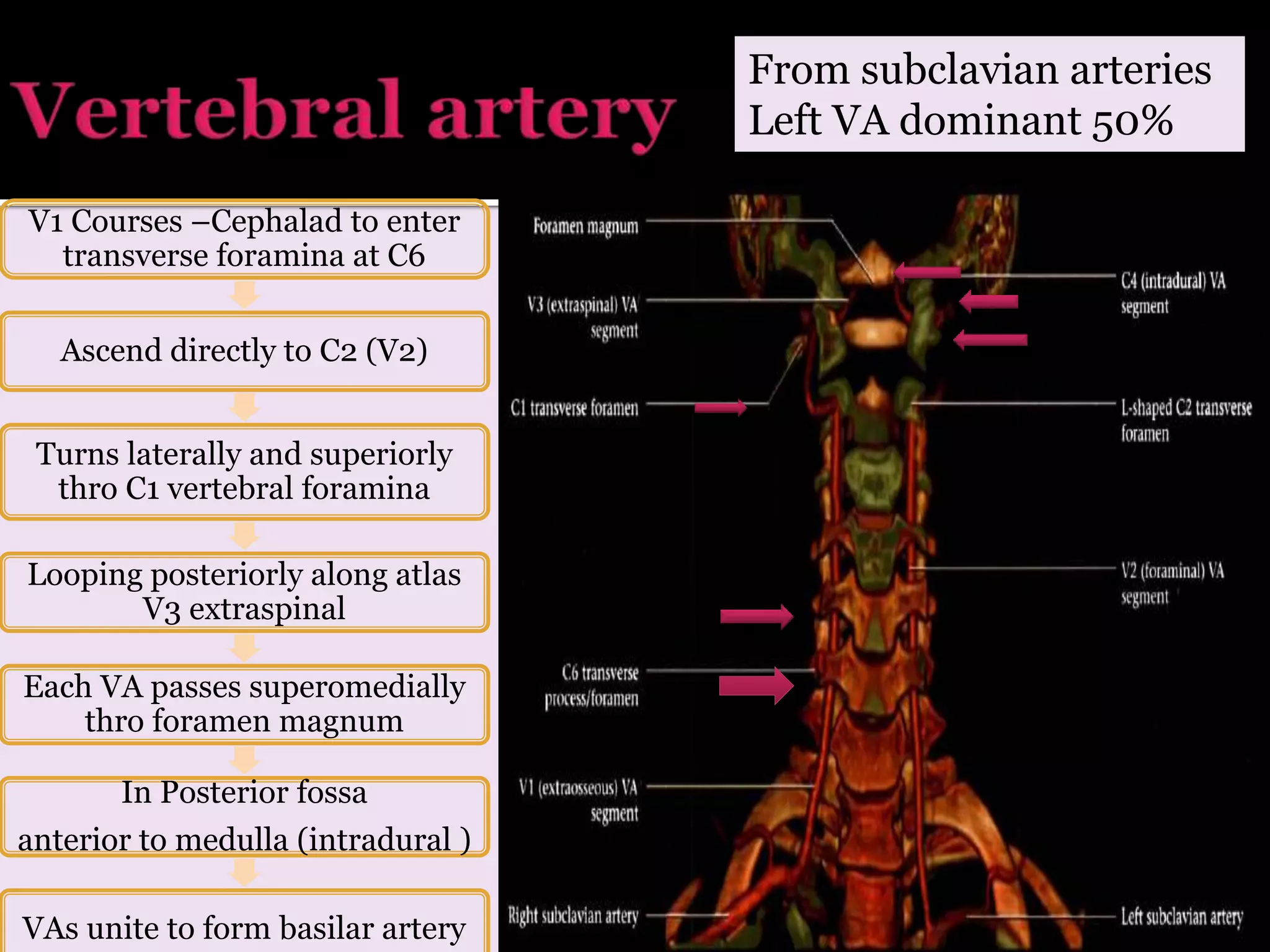
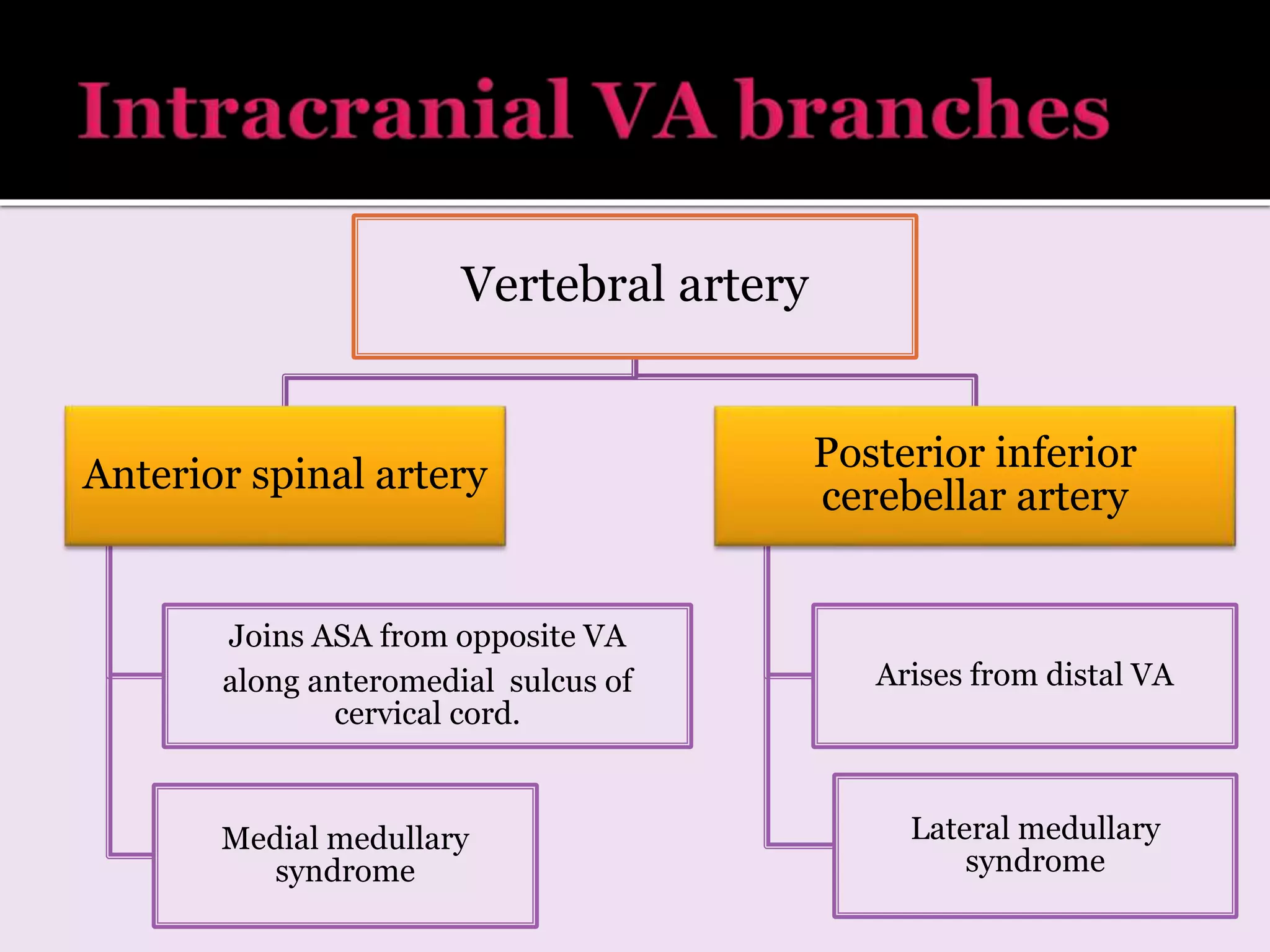
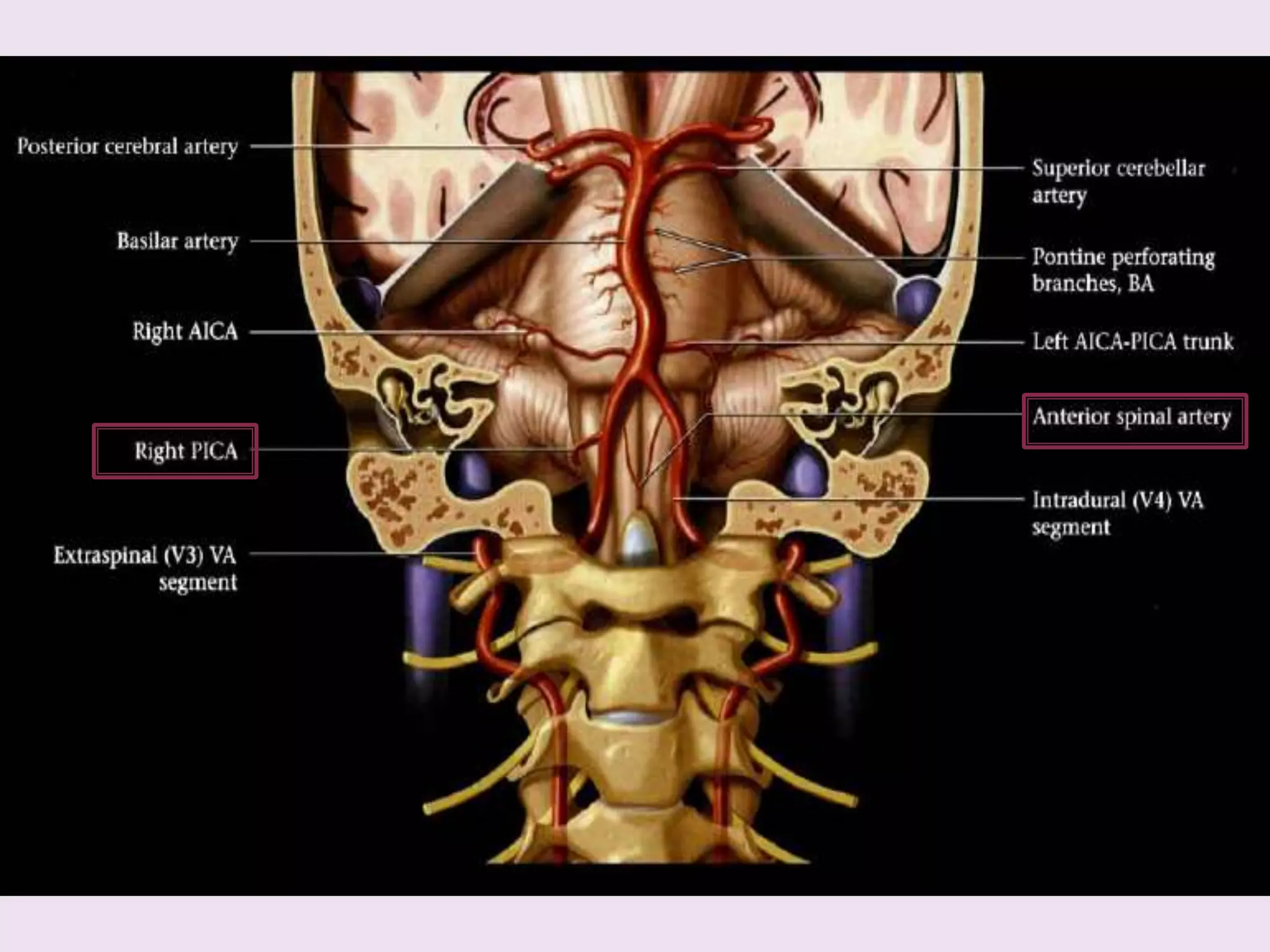
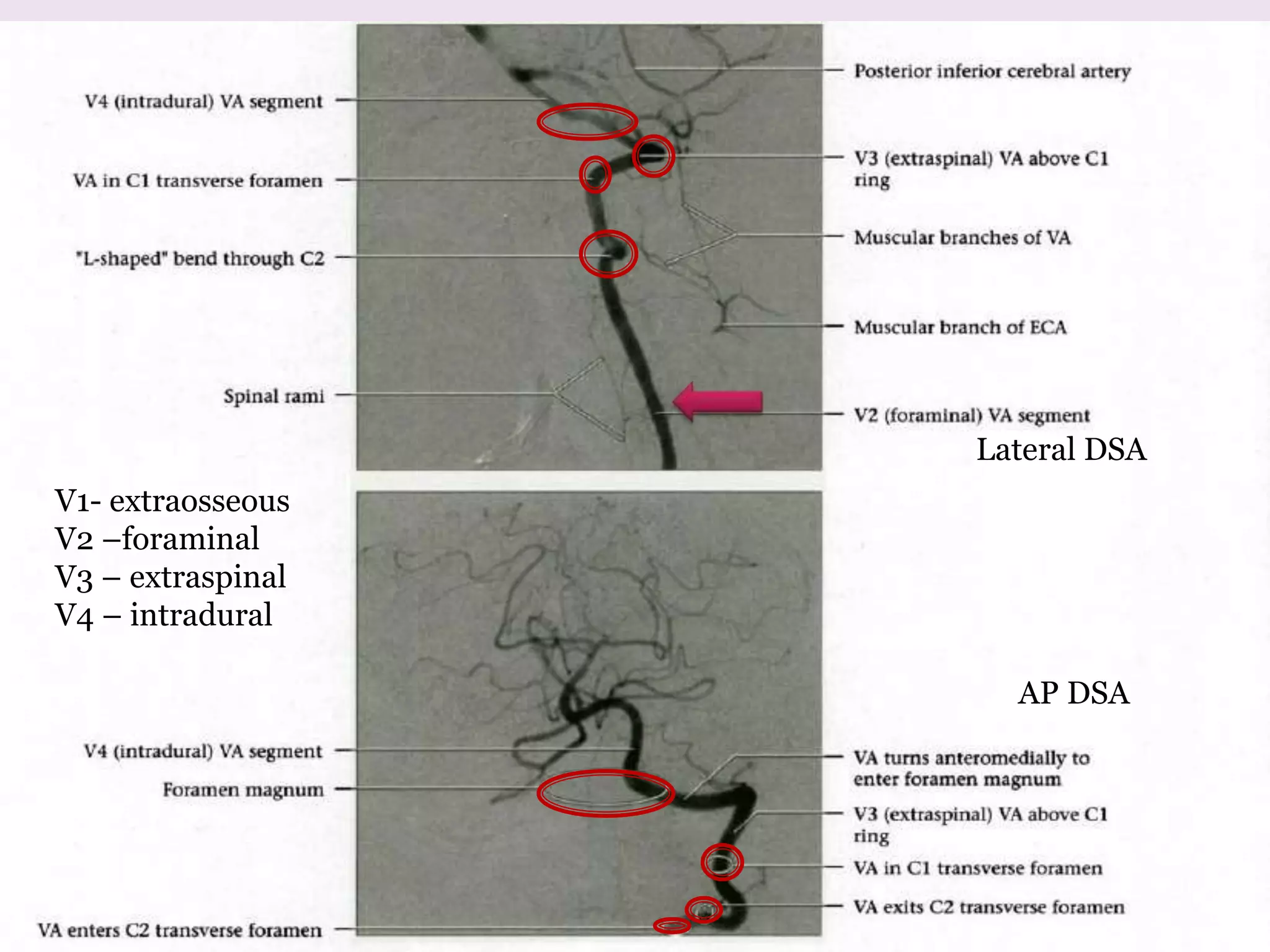
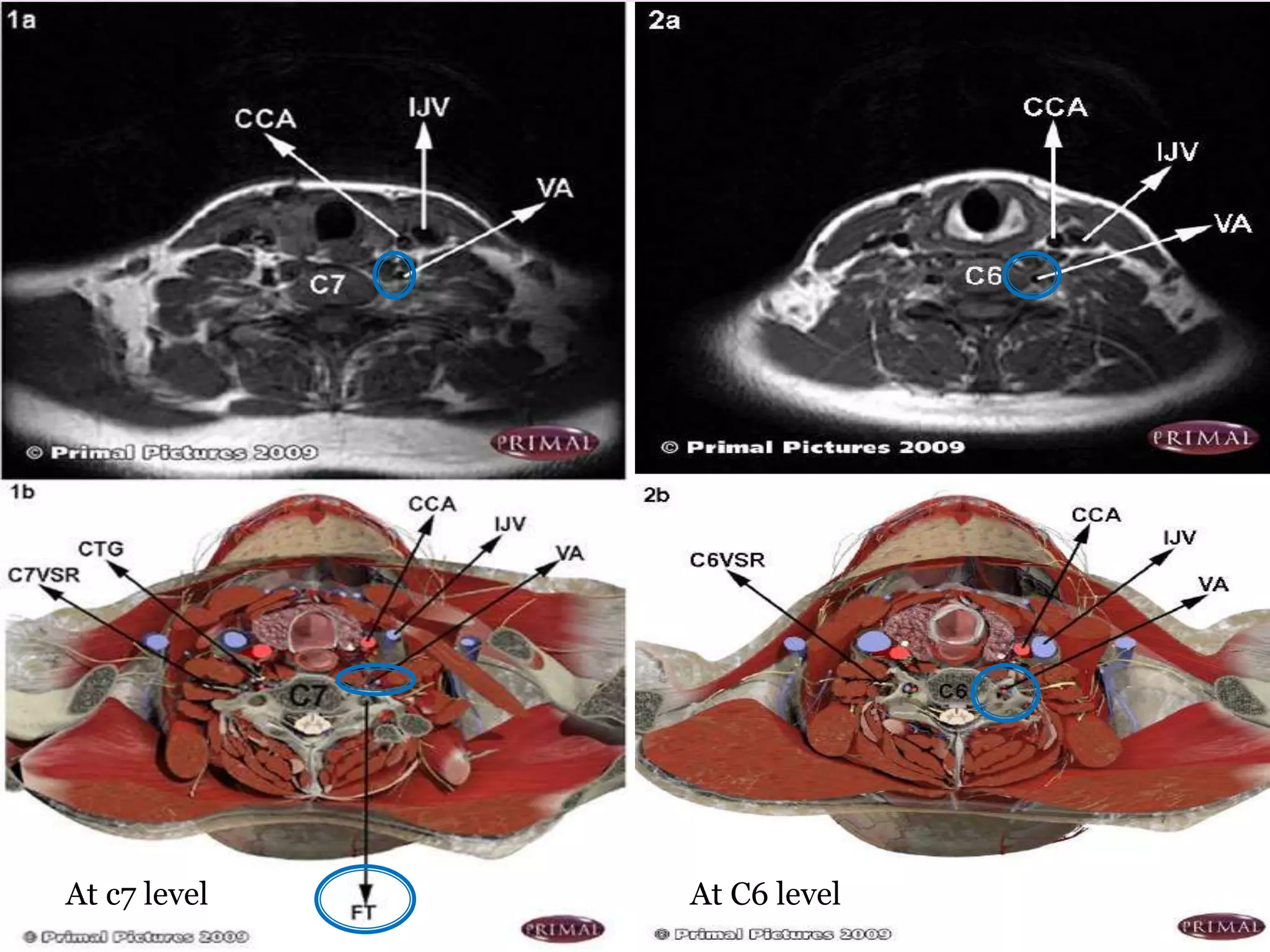
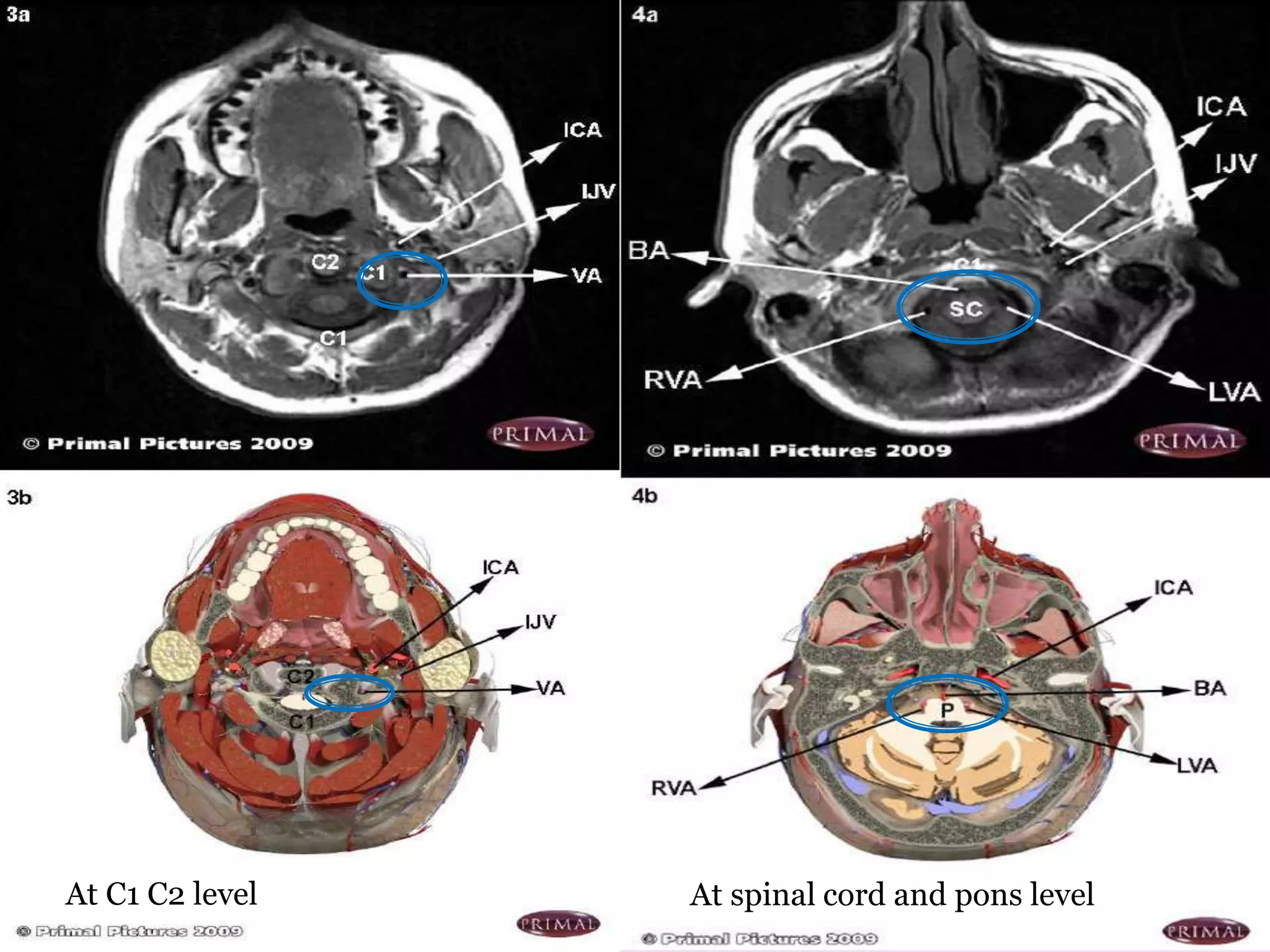
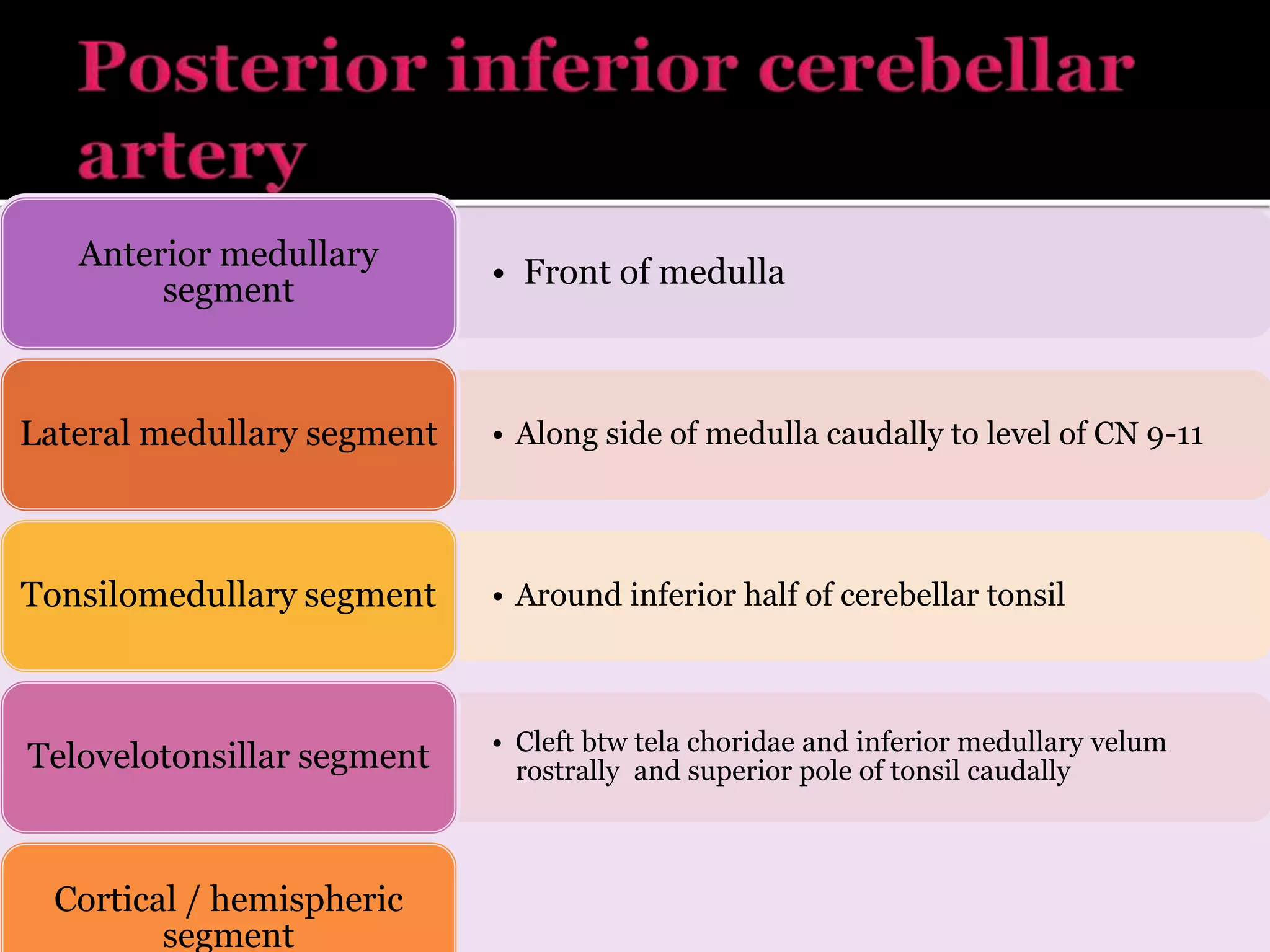
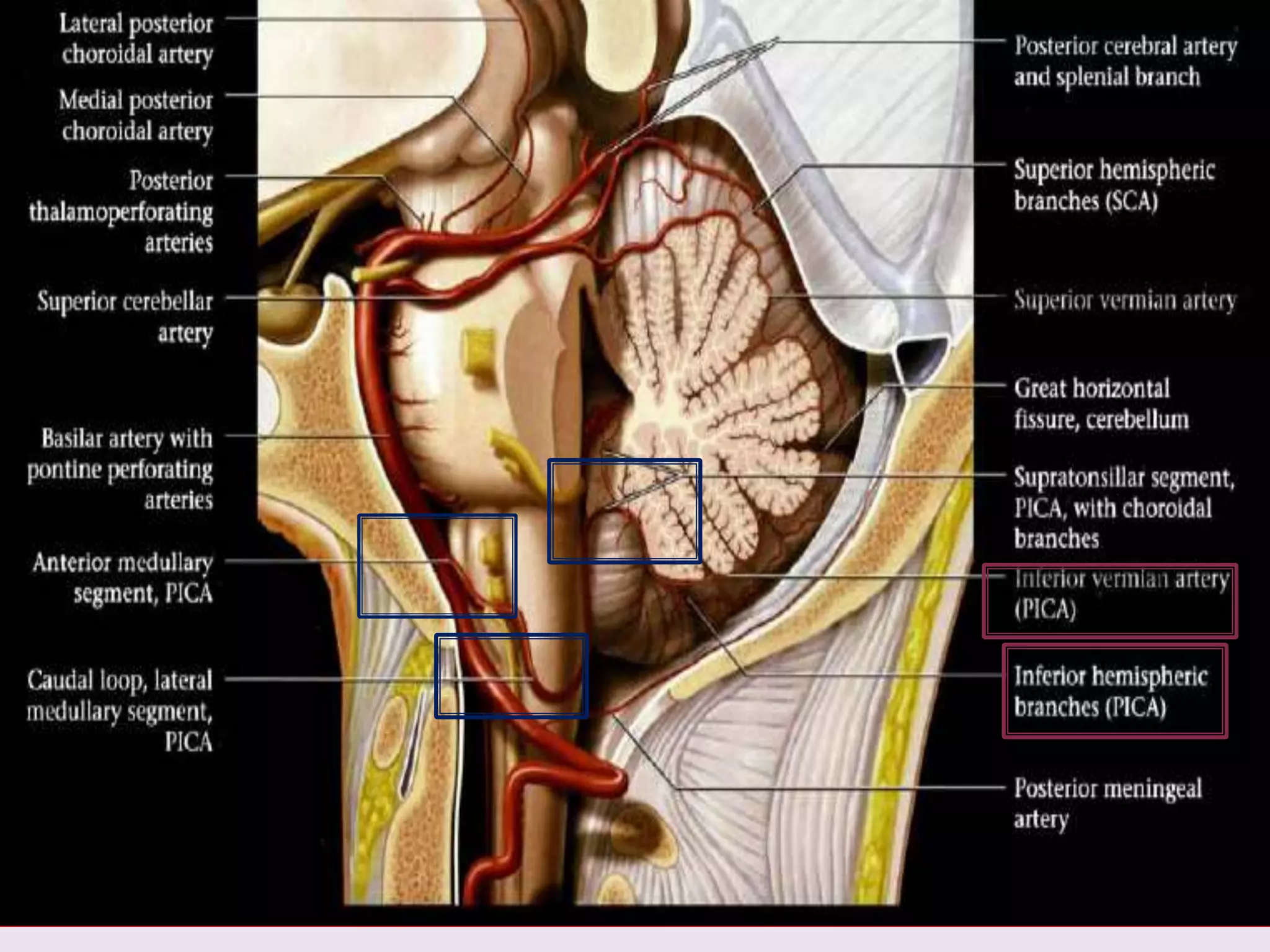
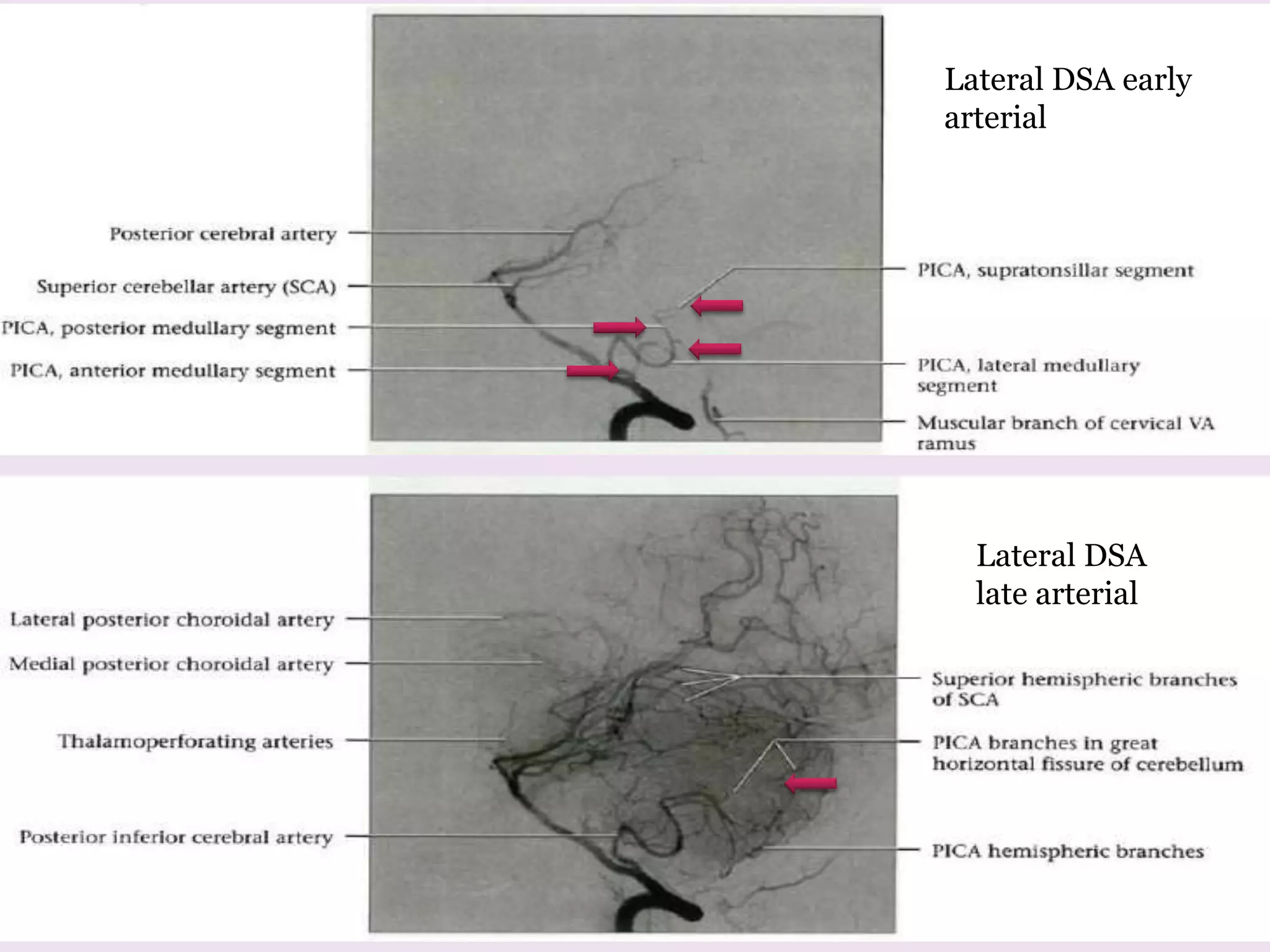
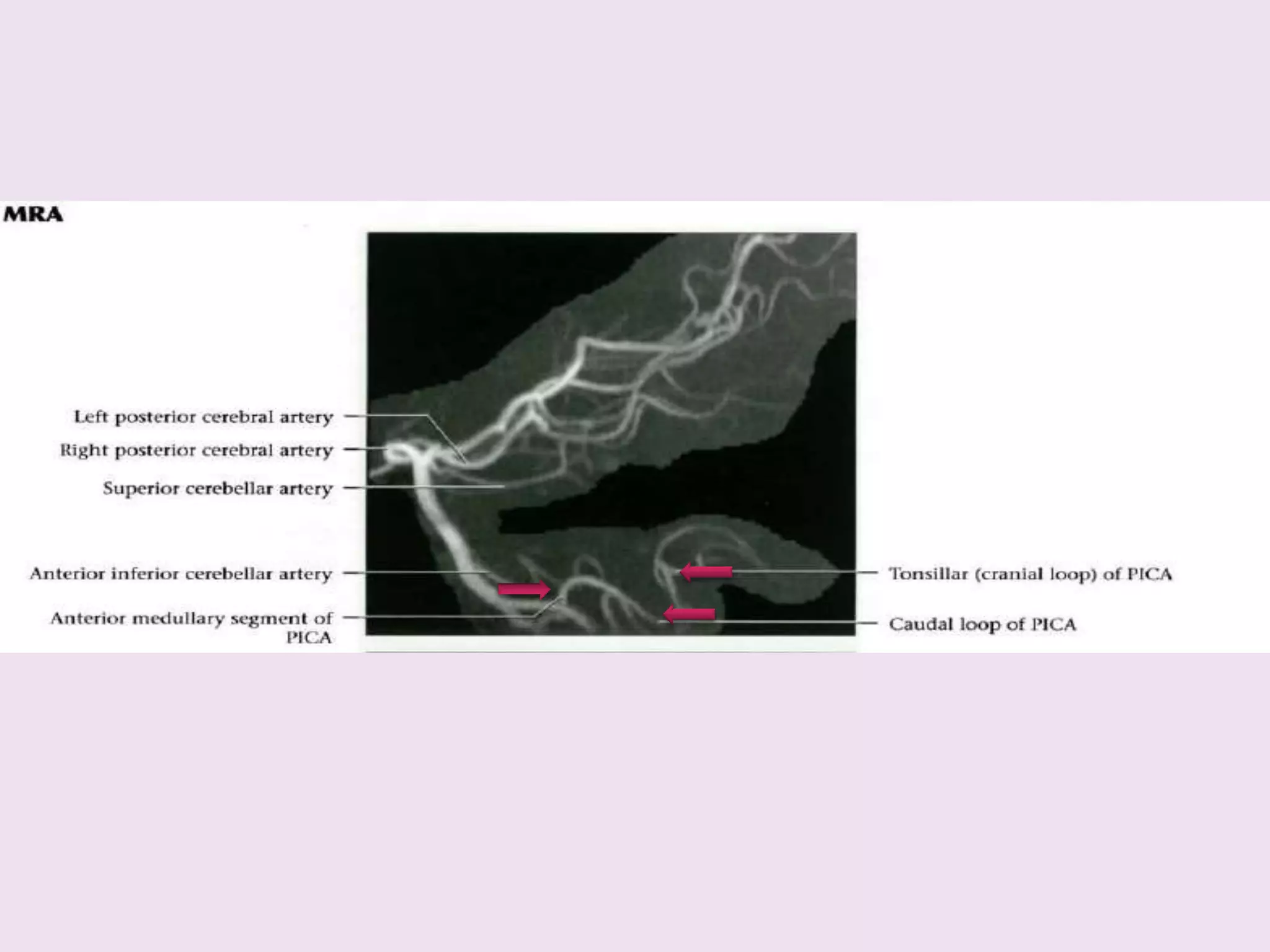
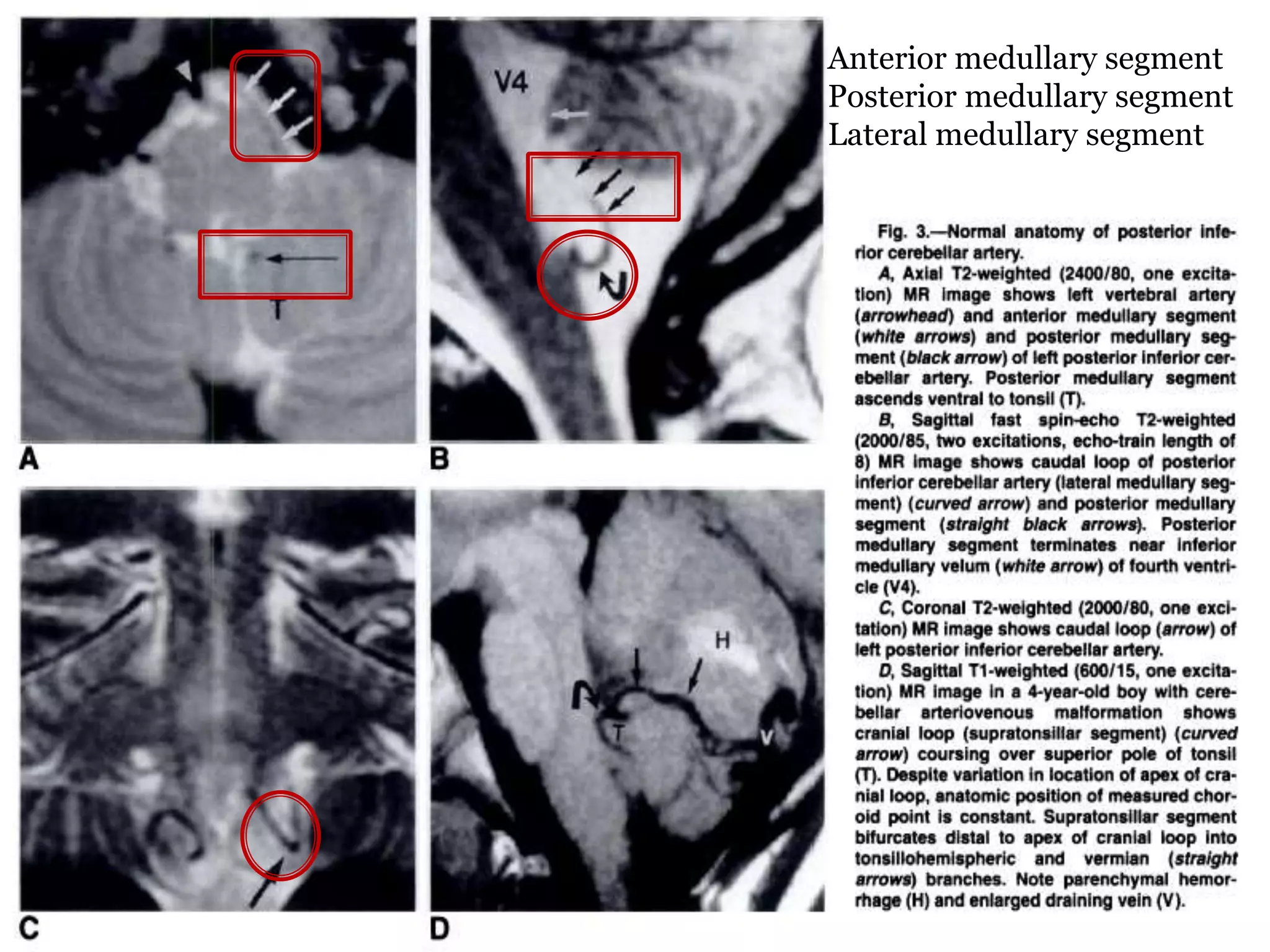
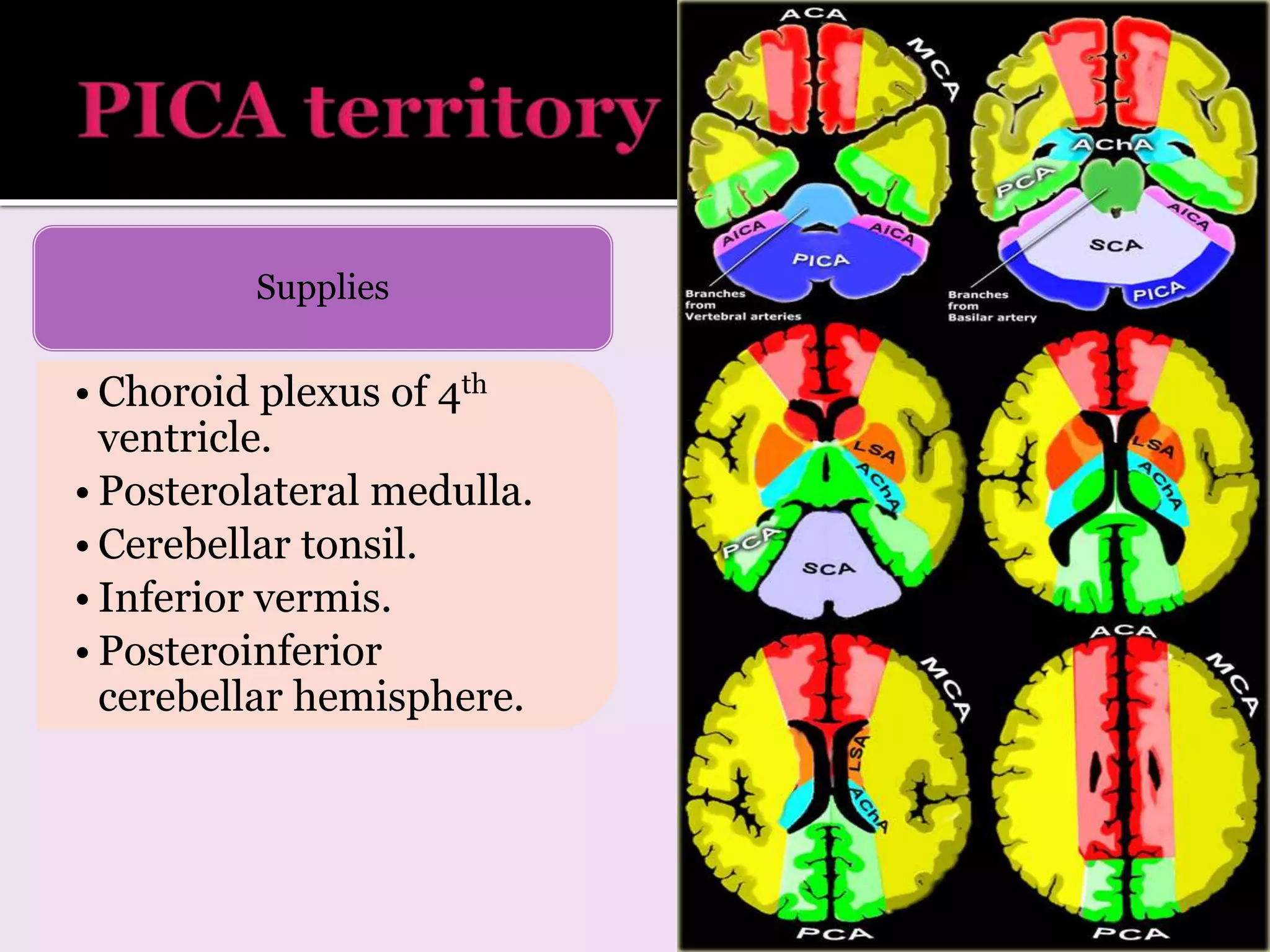
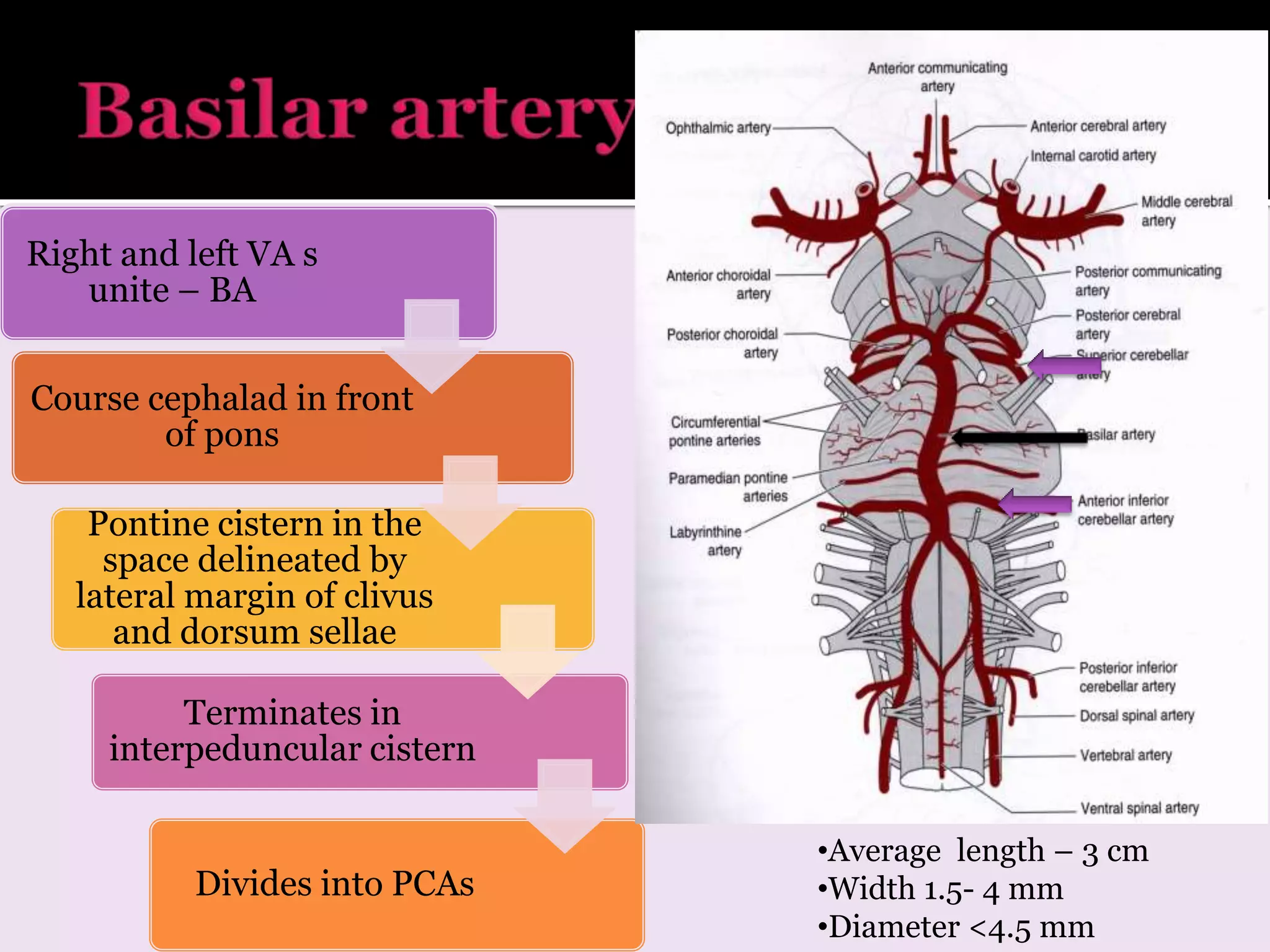
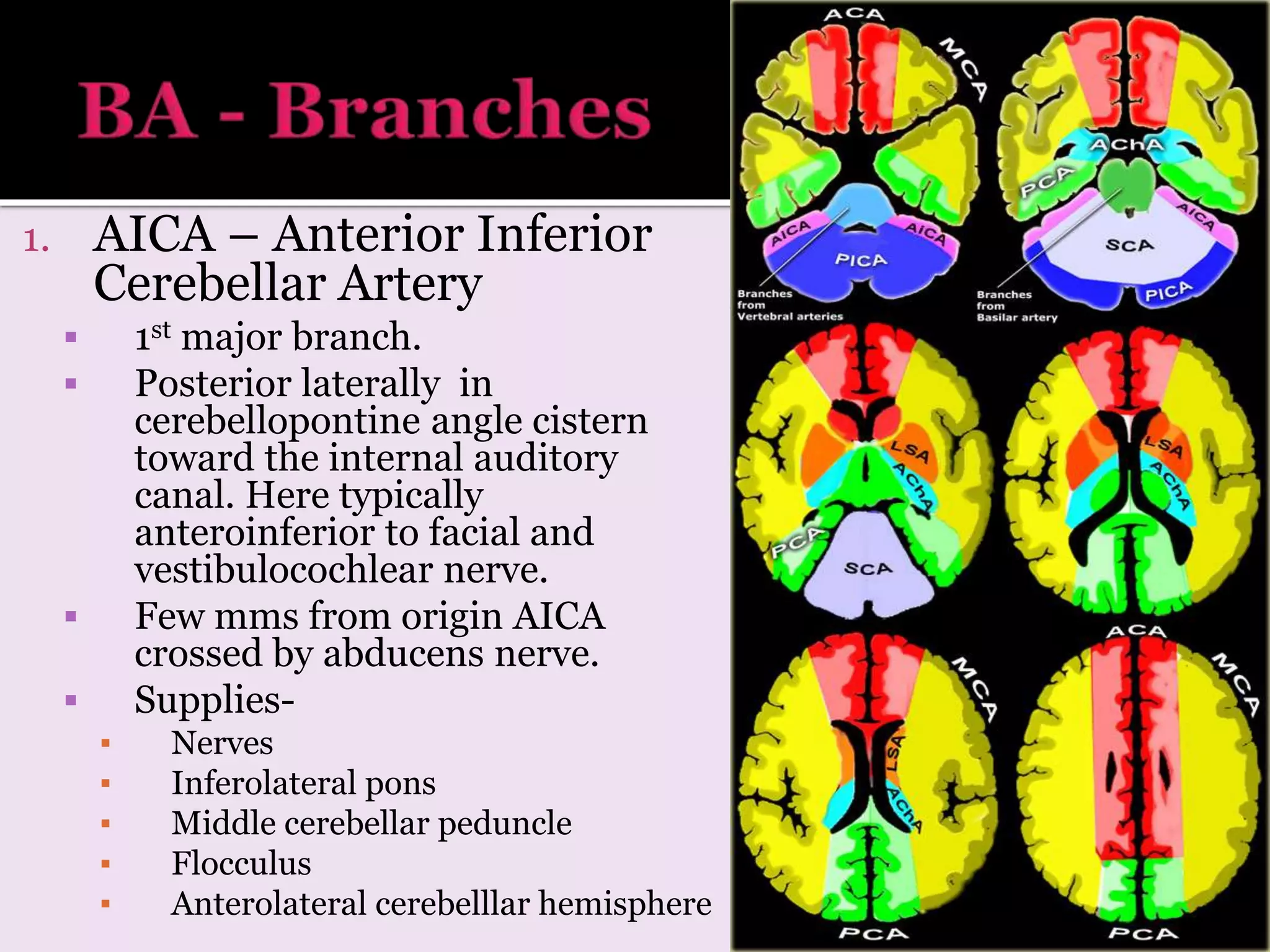
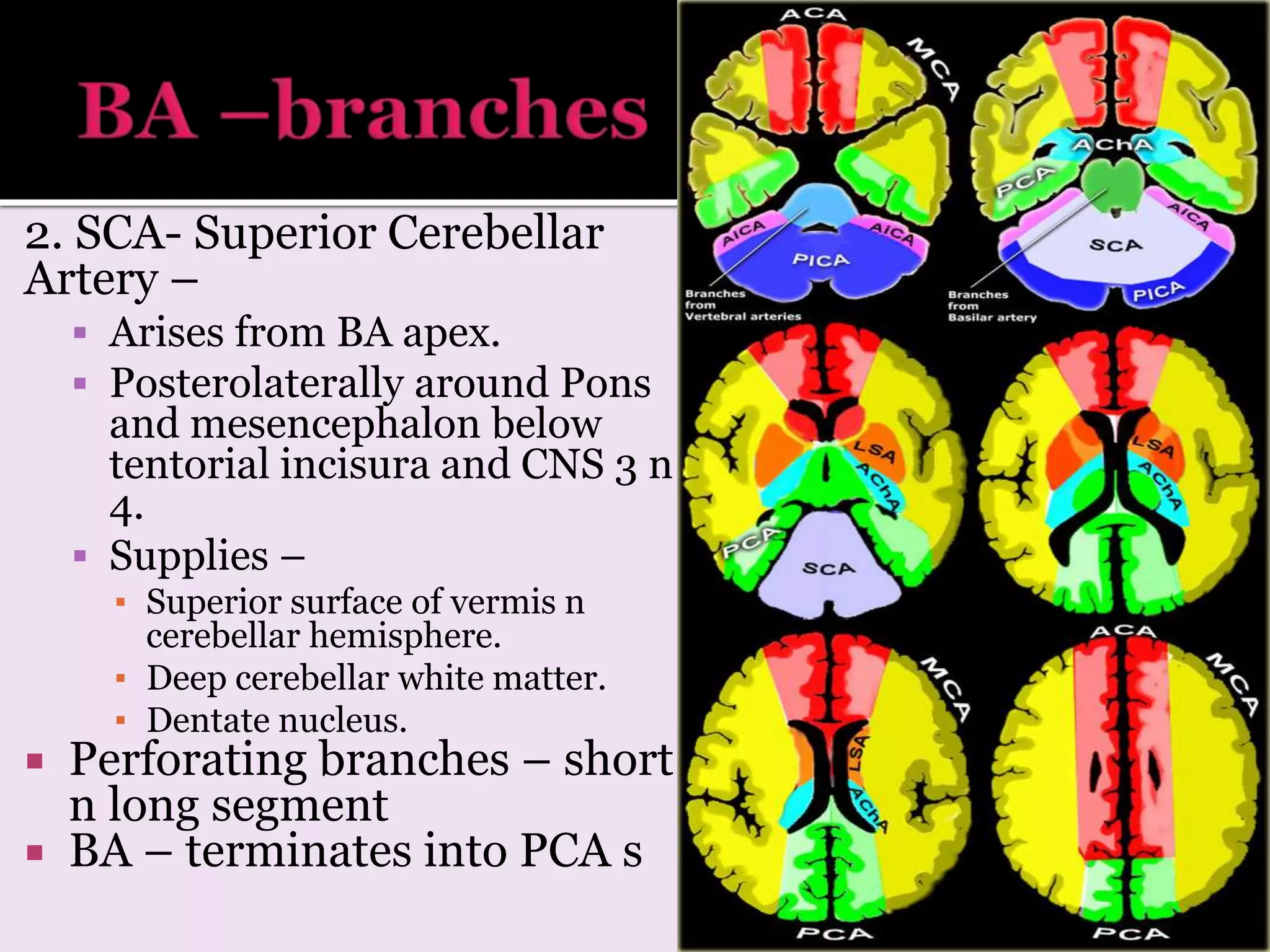
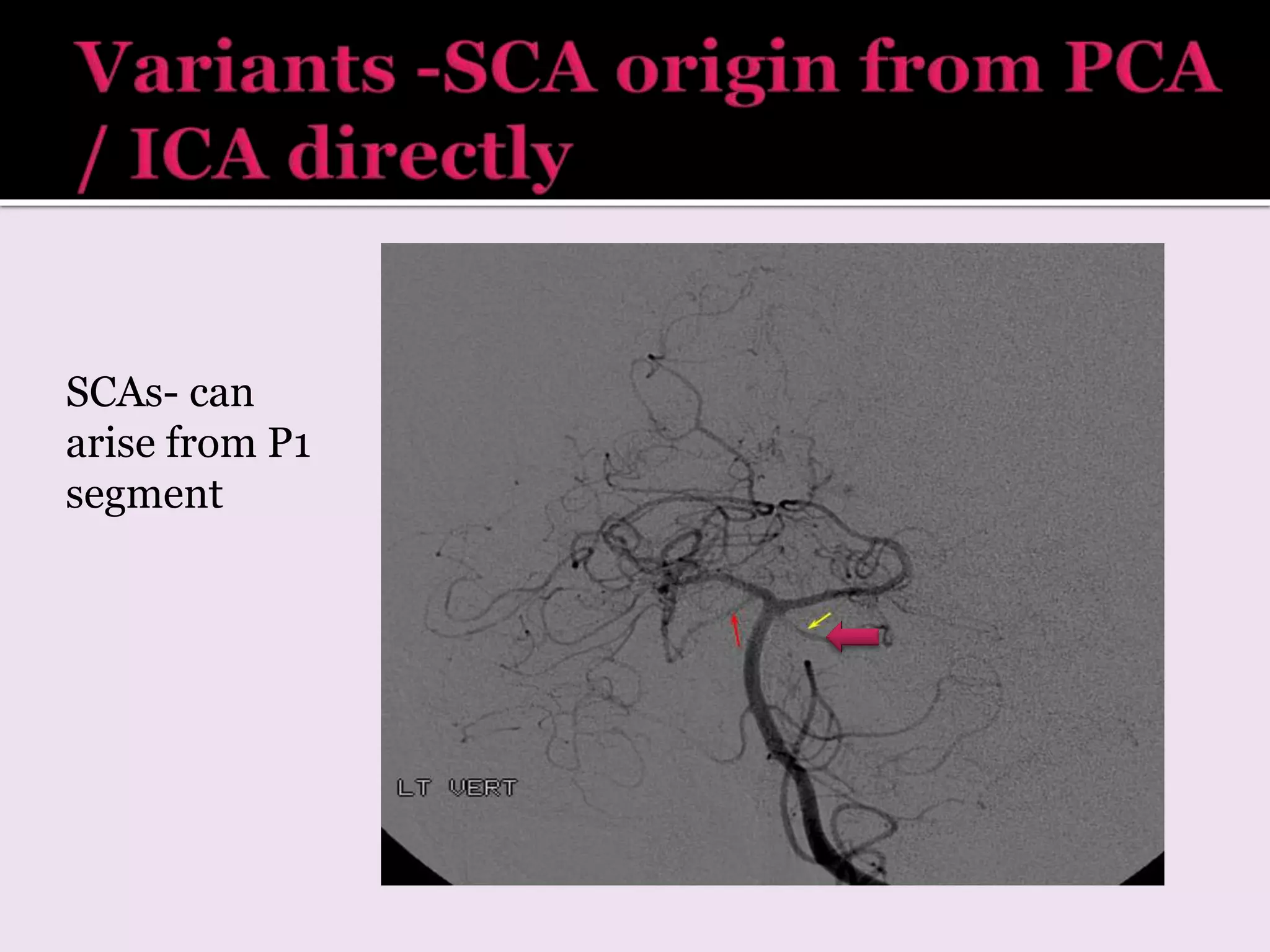
2. It discusses the typical branching patterns and territories supplied by each artery and their segments.
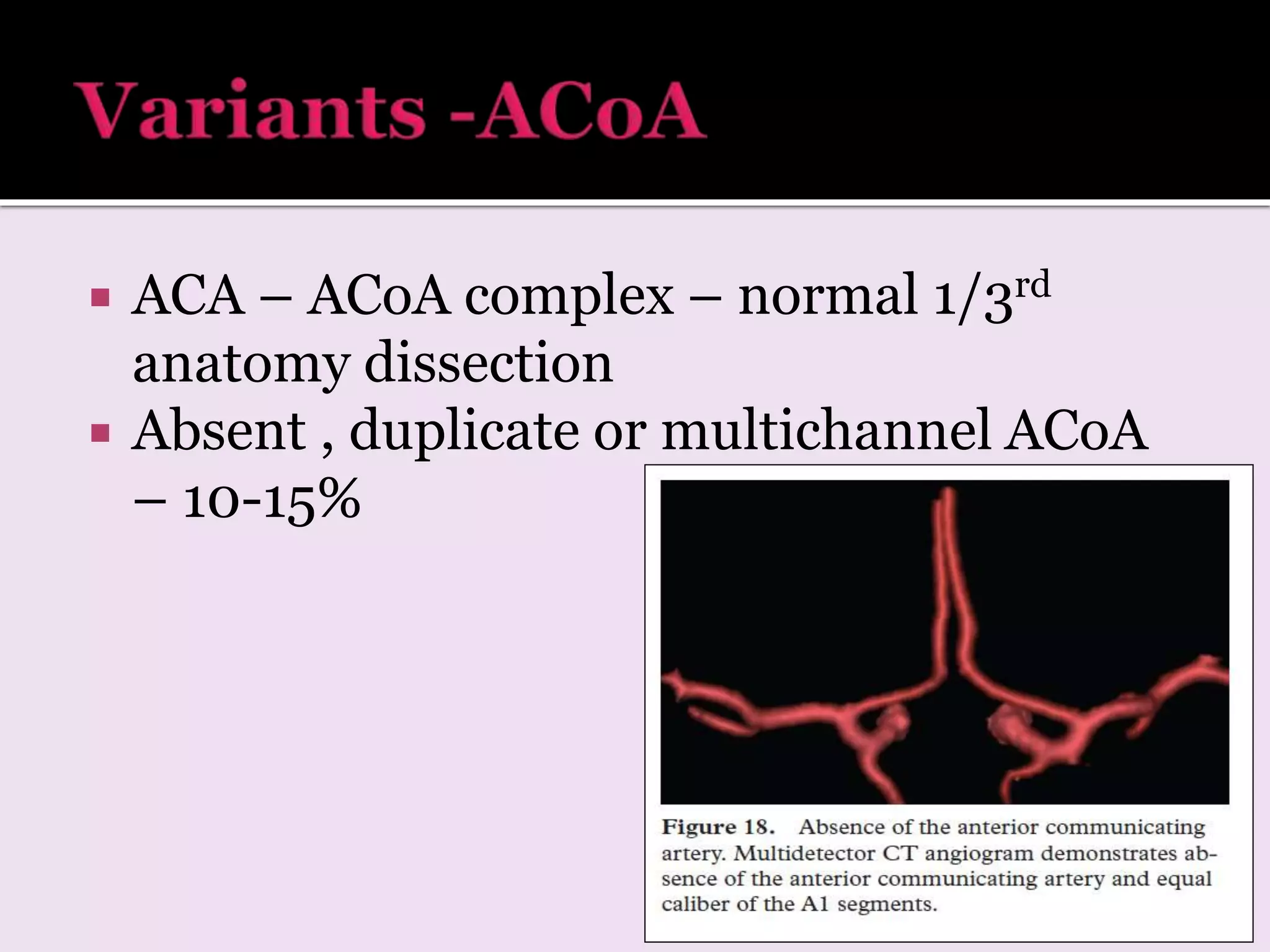
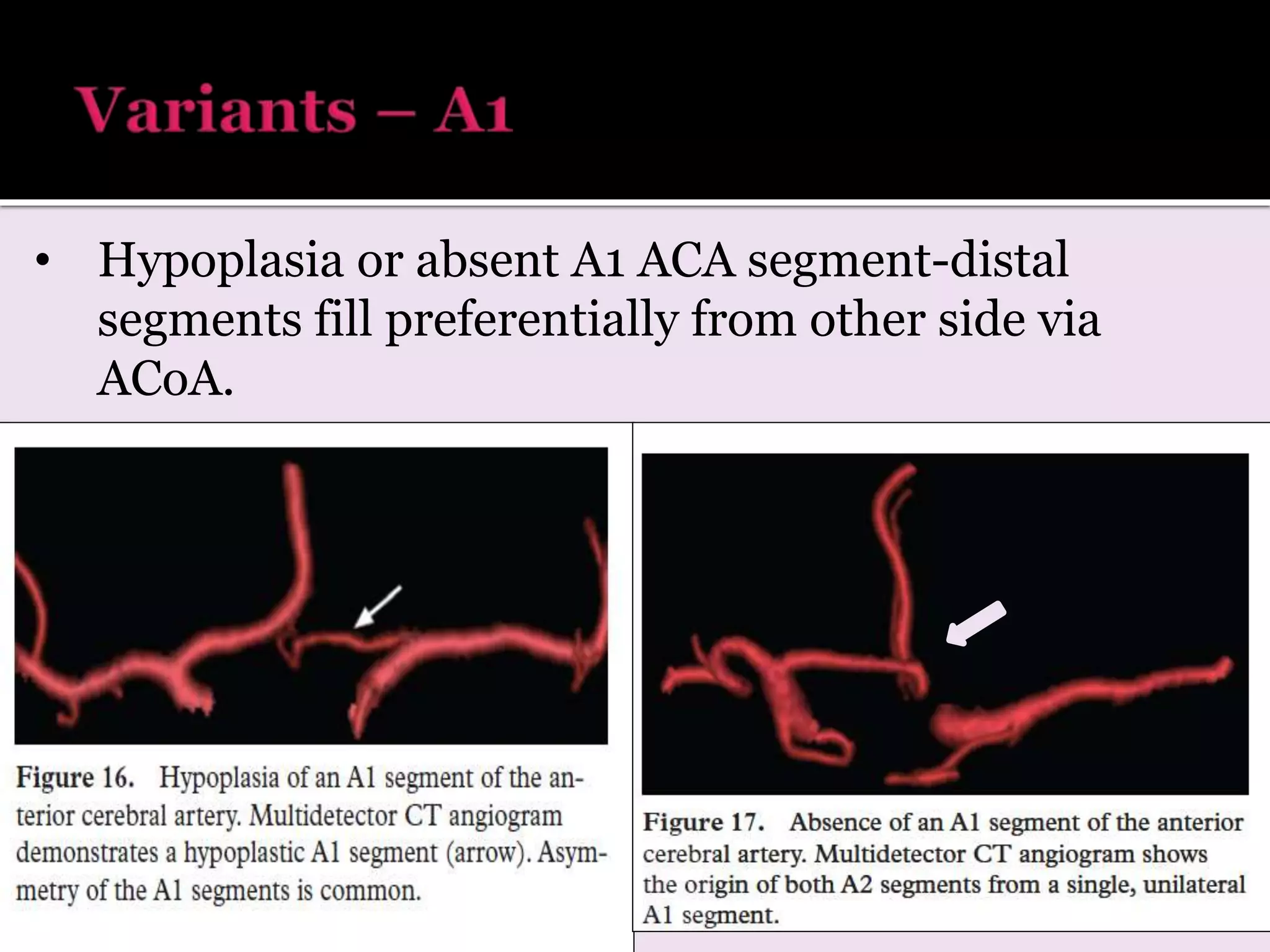
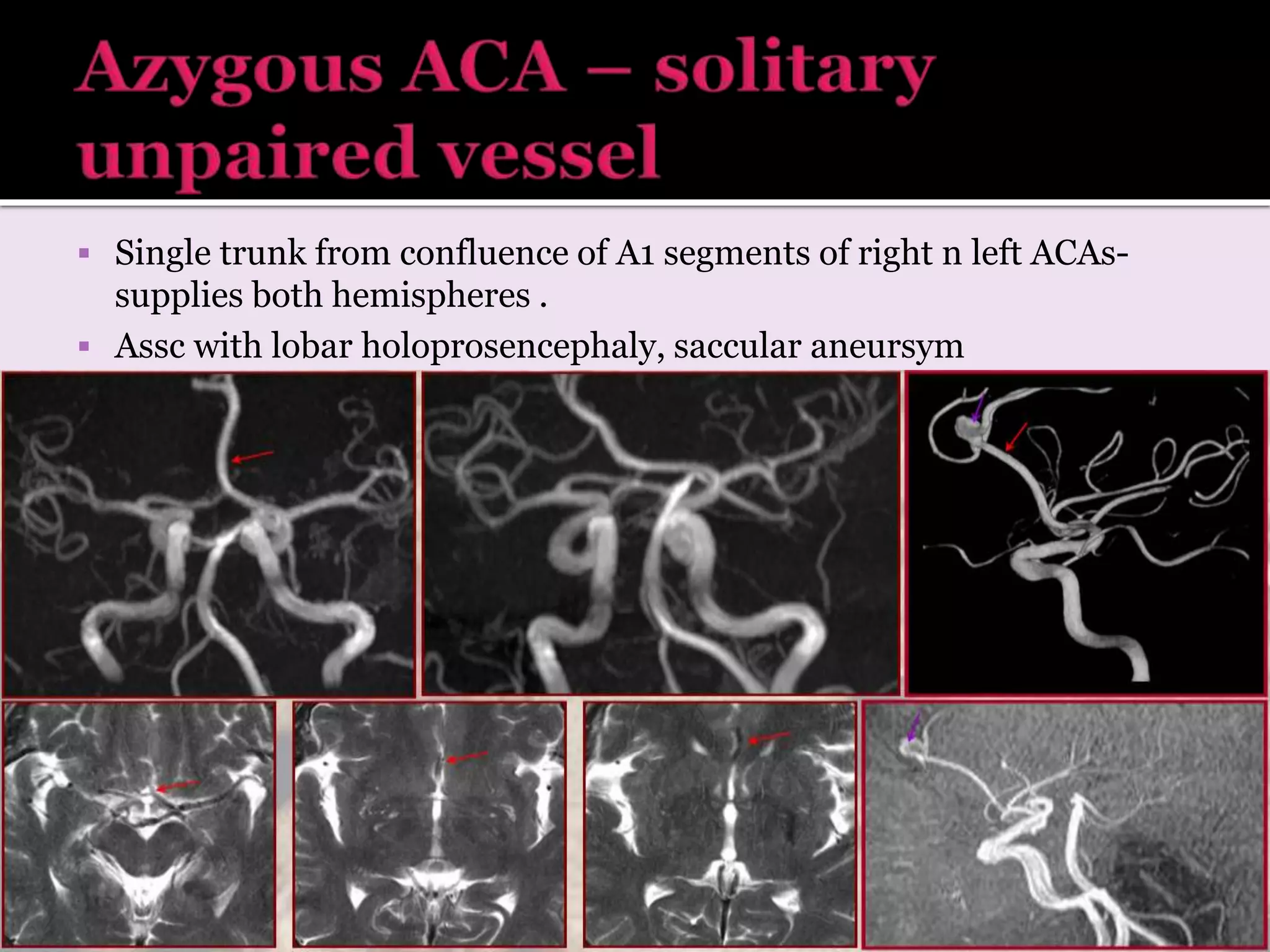
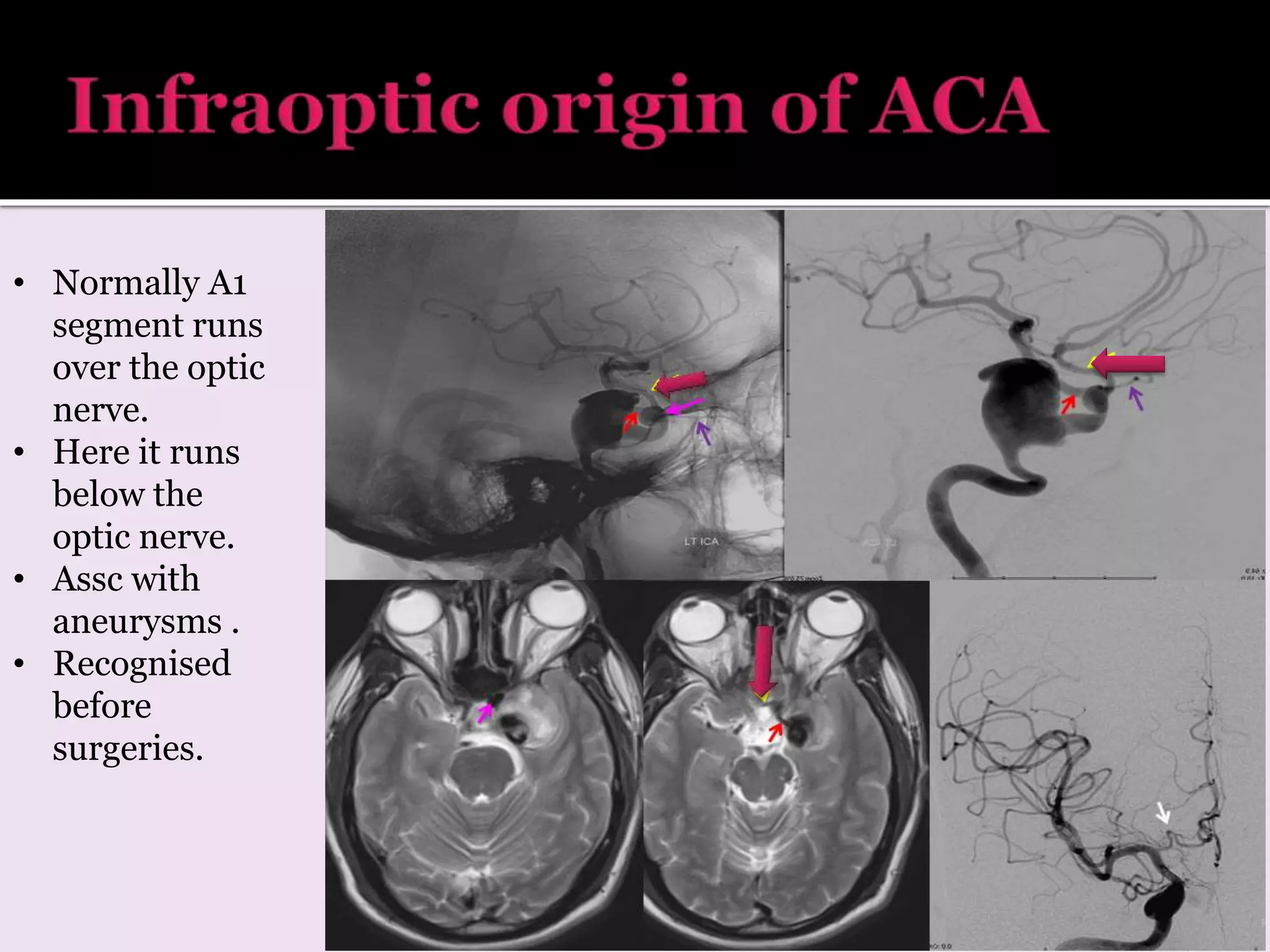
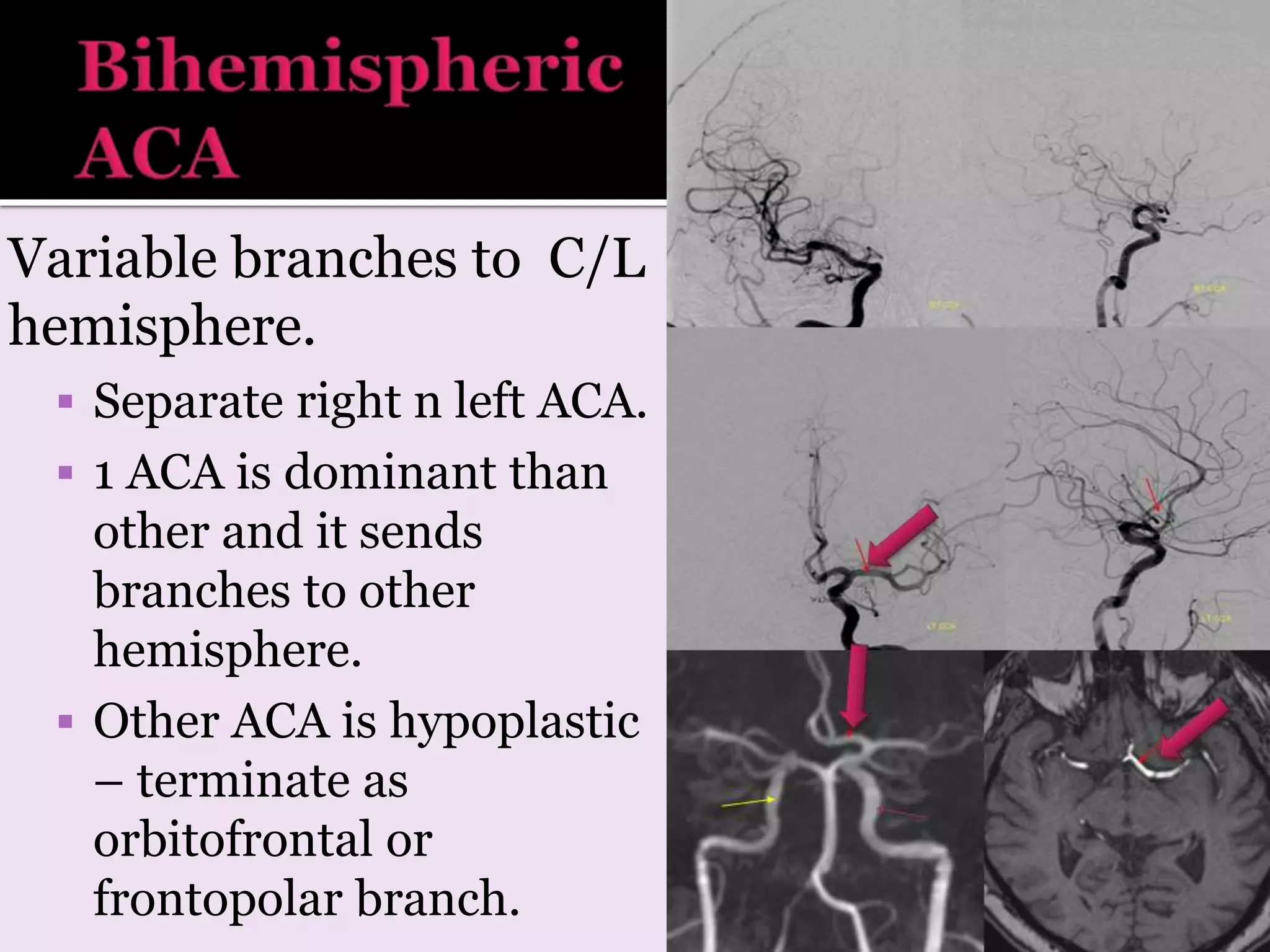
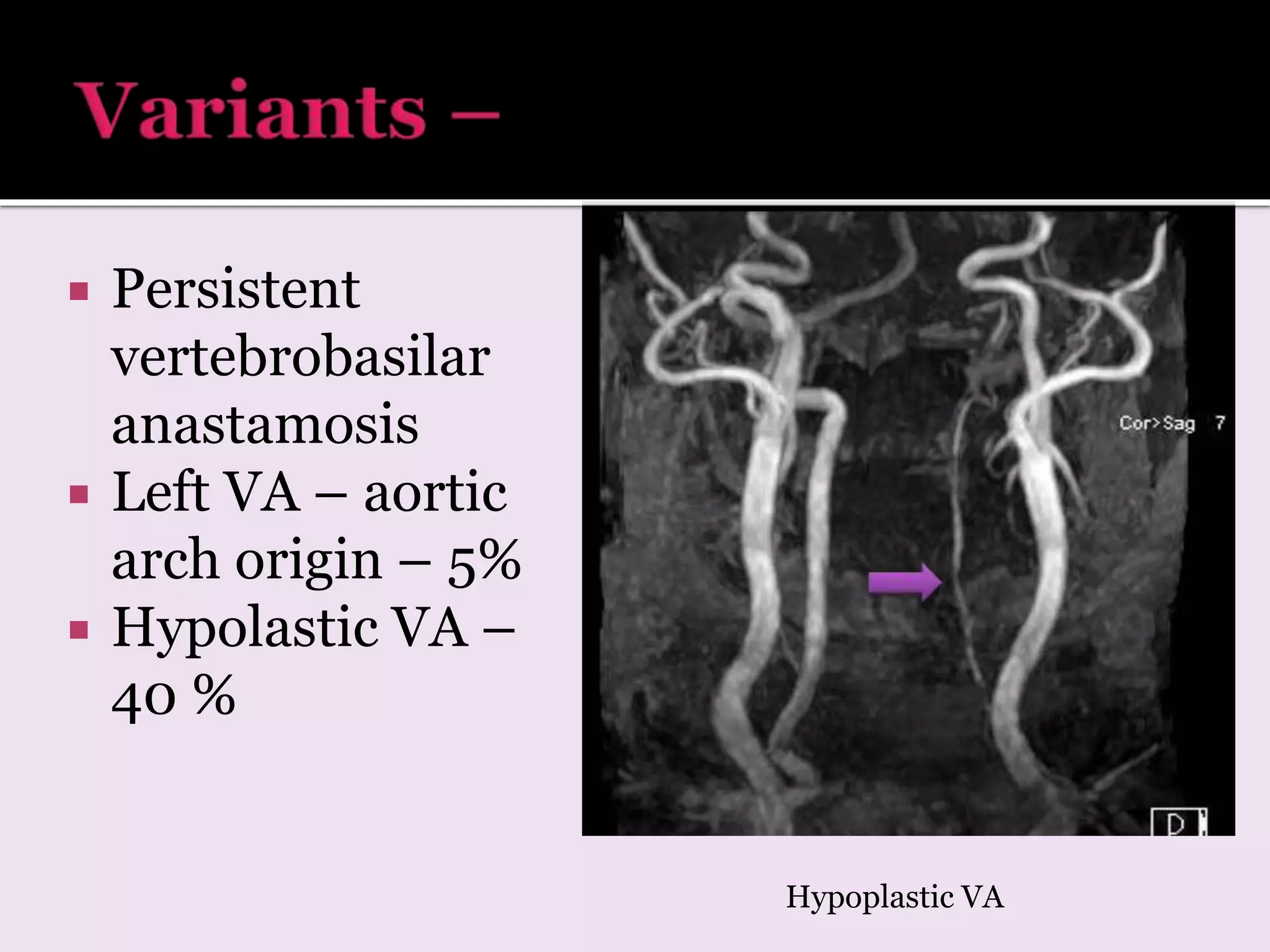
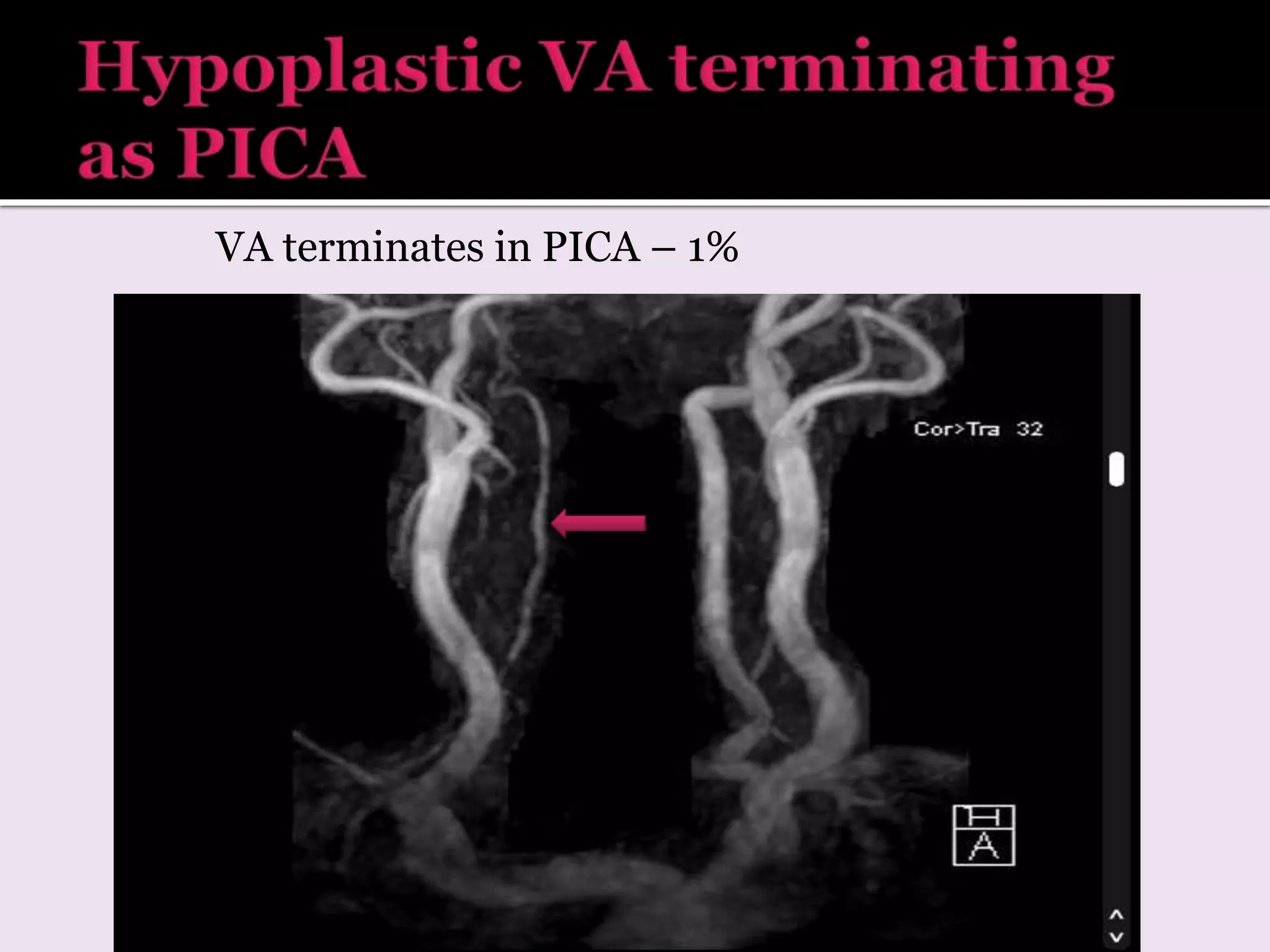
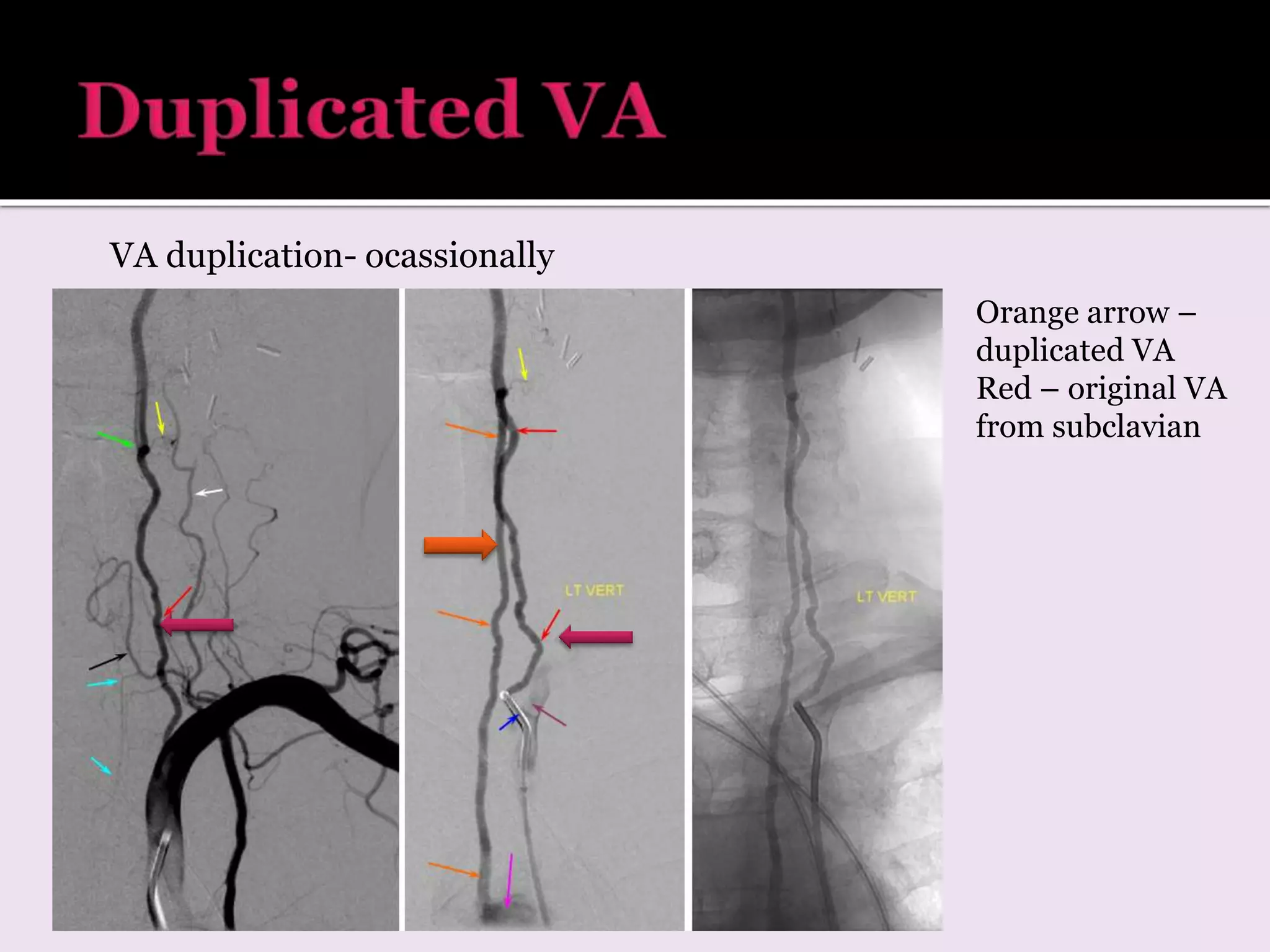
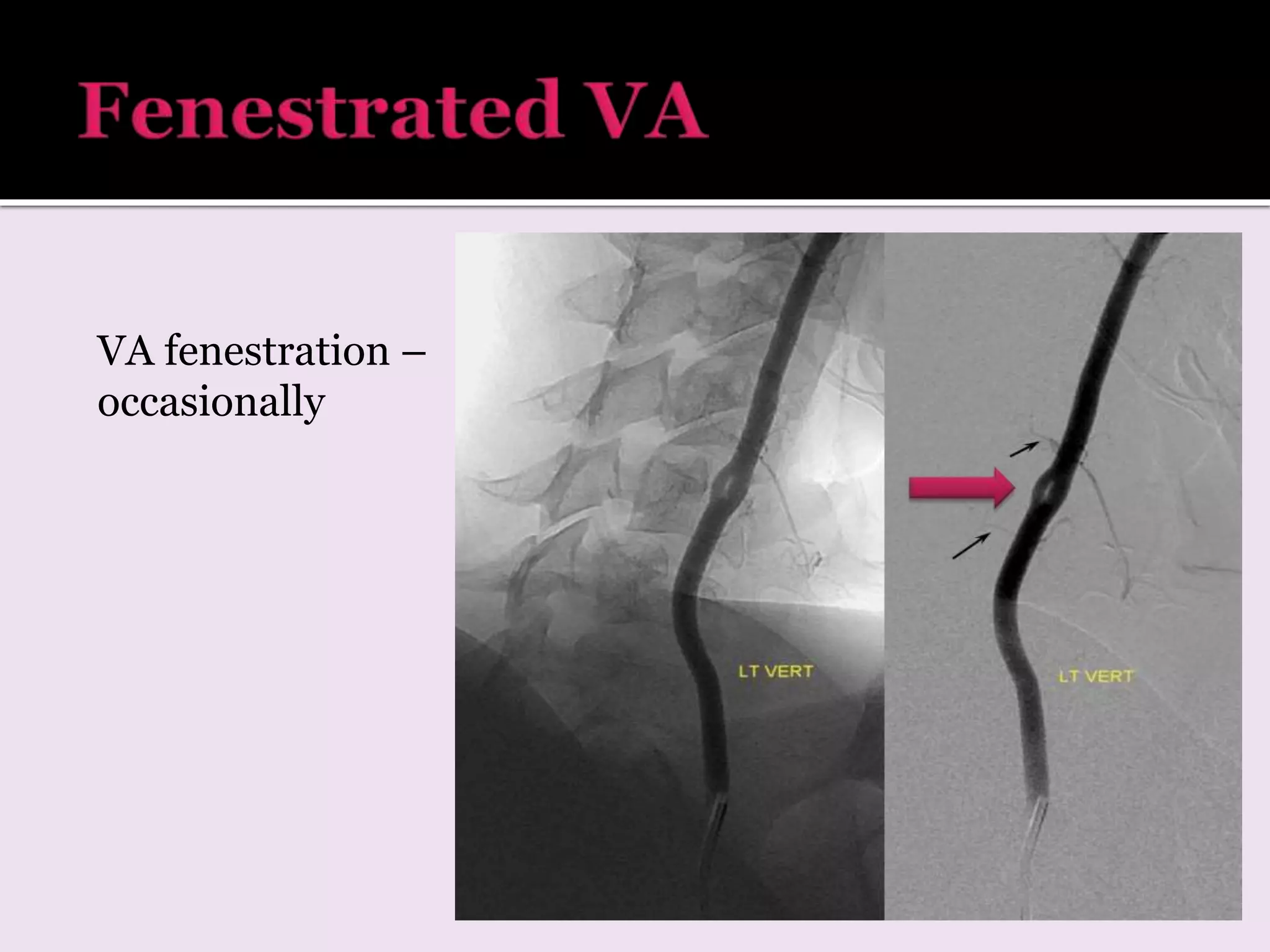
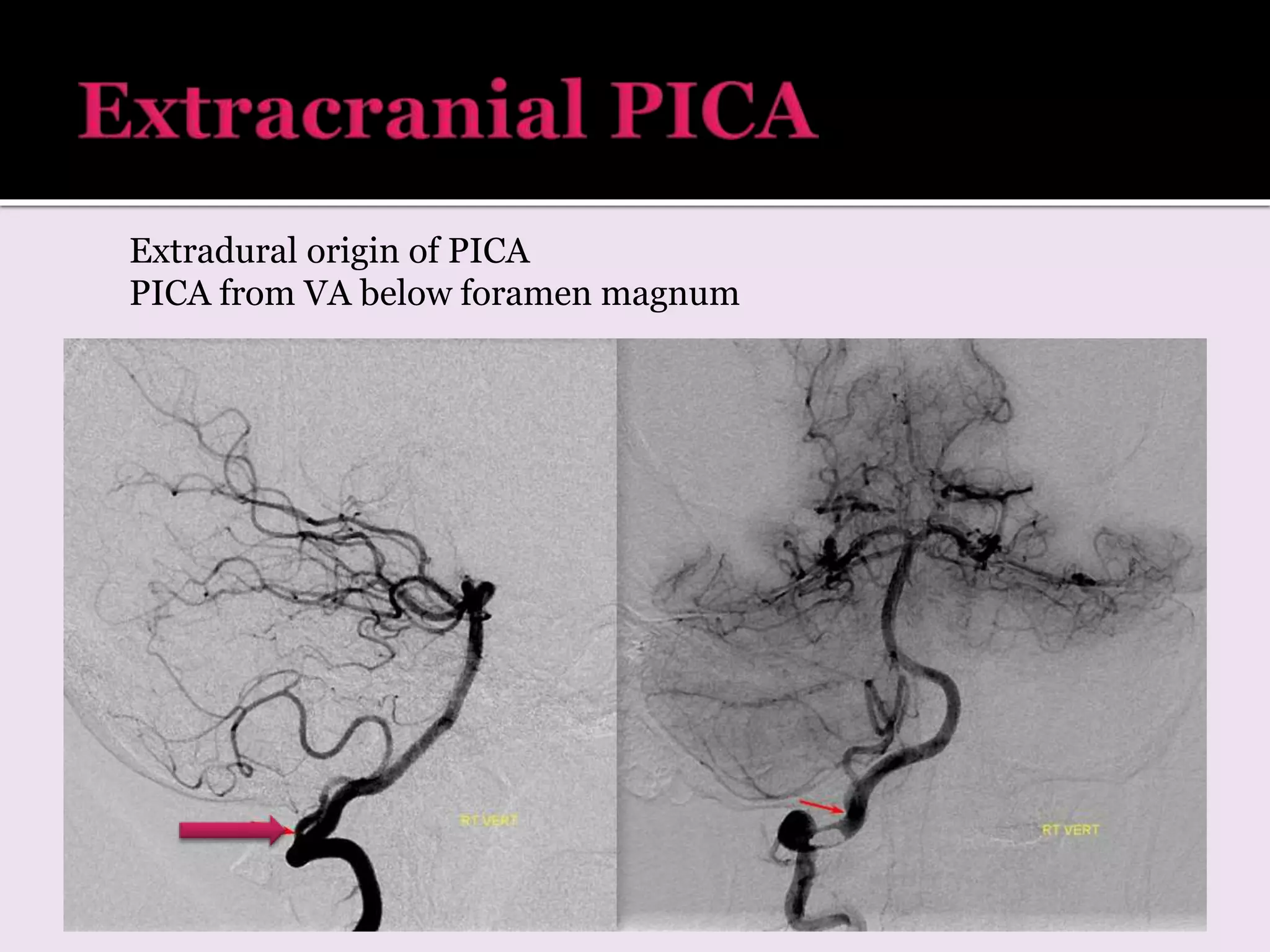
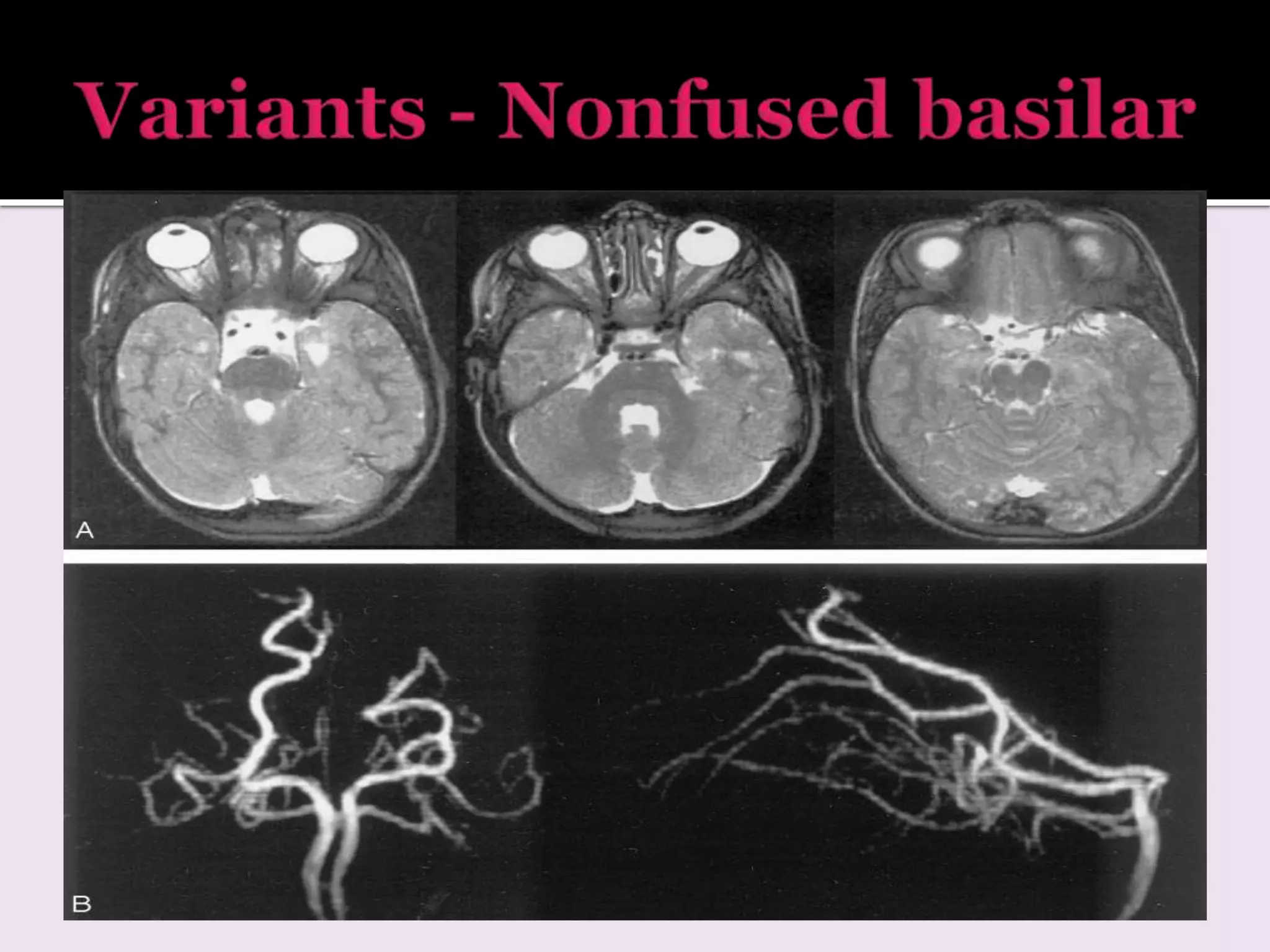
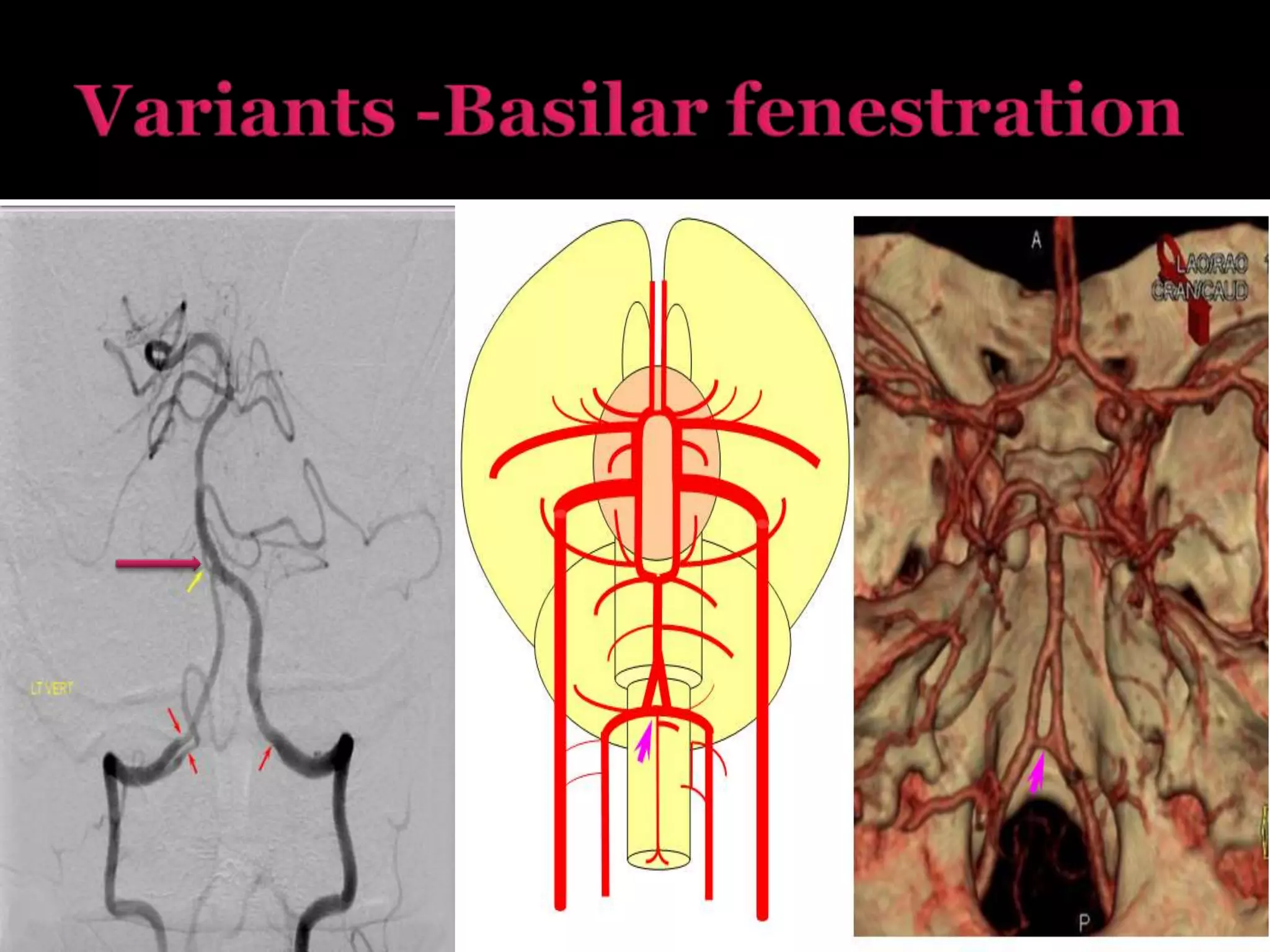
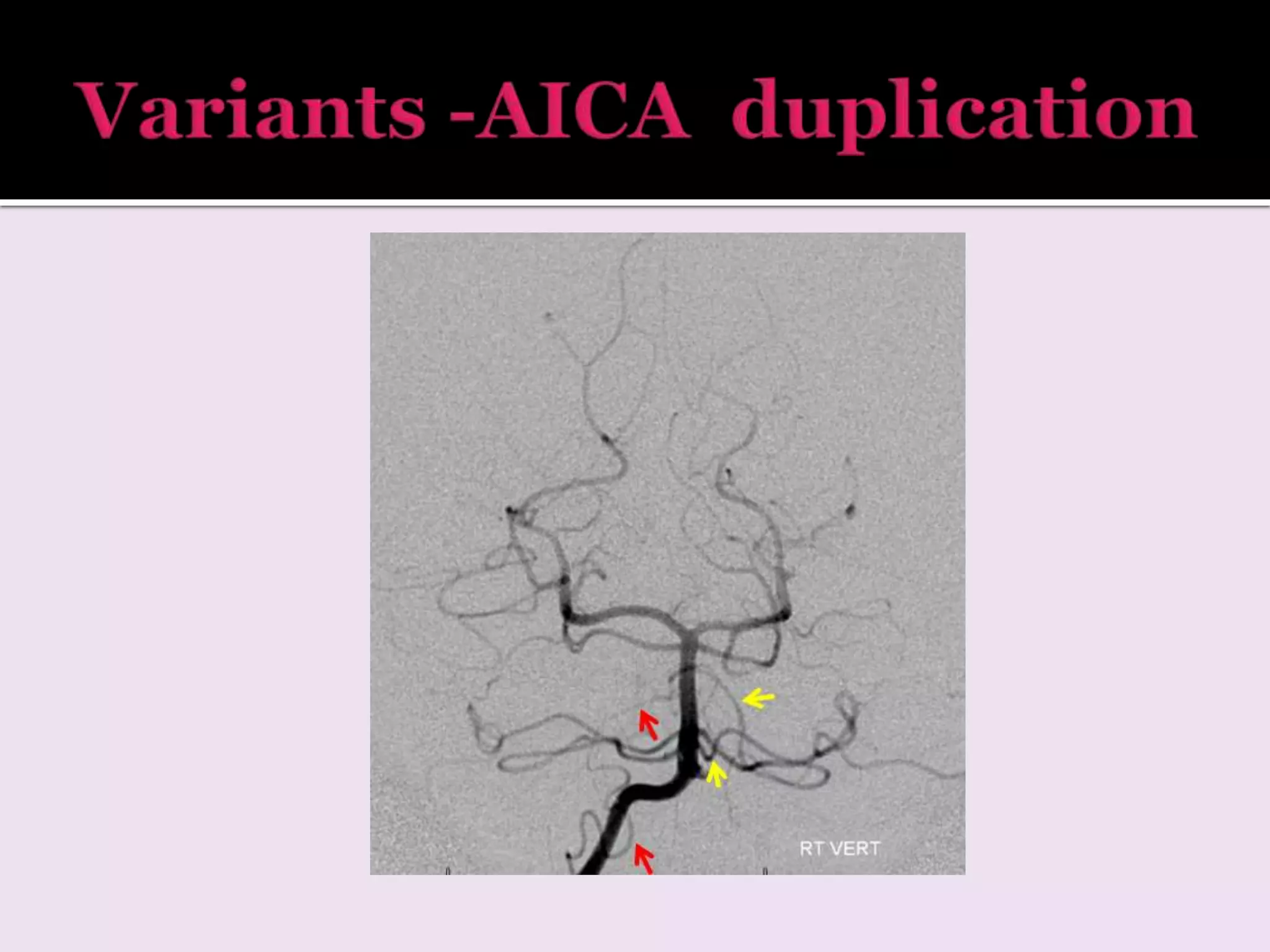
3. Variations in arterial anatomy are also summarized such as fenestrations, duplications, hypoplasia.