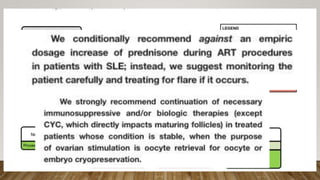
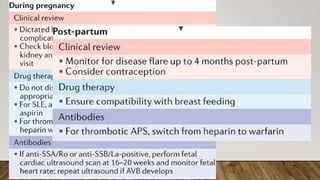
The document discusses management of rheumatic diseases during pregnancy. It notes that remission of the rheumatic disease leads to healthy child in over 90% of cases. It provides screening recommendations and lists medications that are generally considered safe during pregnancy like hydroxychloroquine and low-dose aspirin. Specific rheumatic diseases like SLE, APS, and vasculitis are discussed in terms of risks during pregnancy and monitoring recommendations. Male fertility is also briefly covered.