1) The document discusses metastatic bone disease, defining it as secondary malignant neoplastic disease resulting from metastasis of a primary tumor to the skeletal system. Common primary sites include breast, lung, thyroid, kidney, and prostate.
2) Metastatic bone lesions can be osteolytic or osteoblastic. Osteolytic lesions result from tumor-secreted PTHrP stimulating bone resorption and a "vicious cycle".
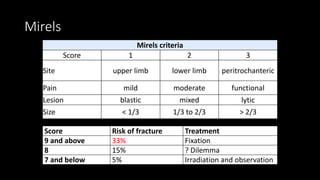
3) Management is multidisciplinary, with goals of pain relief, preserving function, and maximizing quality of life. Treatment may include radiotherapy, chemotherapy, bisphosphonates, surgery, or a combination depending on prognosis, based on scoring systems like Tokuhash