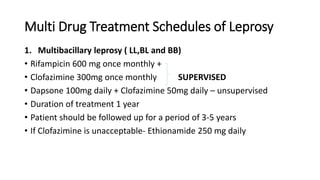
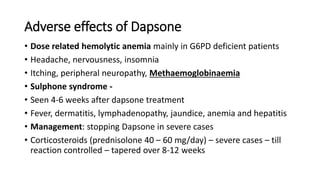
This document discusses drugs used to treat leprosy, including dapsone, clofazimine, rifampicin, and ethionamide. It describes the classification of leprosy as paucibacillary or multibacillary and the corresponding multi-drug treatment schedules recommended by the WHO. Adverse effects and alternative regimens are also covered. The document concludes by emphasizing compassion for leprosy patients and the importance of rehabilitation programs.