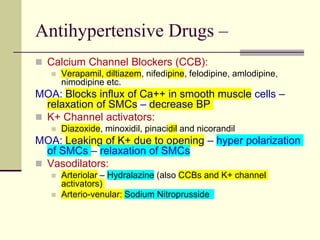
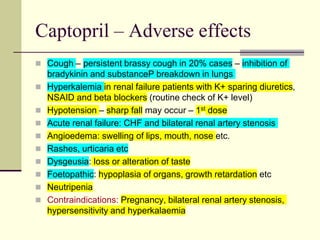
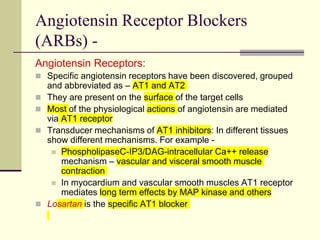
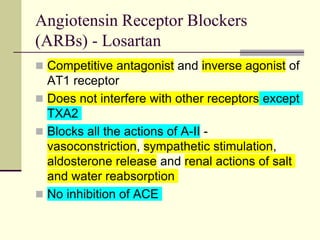
This document discusses various classes of drugs used to treat hypertension. It describes the mechanisms of action, effects, and examples of drugs in the following classes: diuretics, ACE inhibitors, angiotensin receptor blockers, beta blockers, calcium channel blockers, and vasodilators. It also provides background on renin-angiotensin system and the physiological role of angiotensin-converting enzyme. Specific drugs discussed in detail include captopril, enalapril, losartan, and metoprolol.