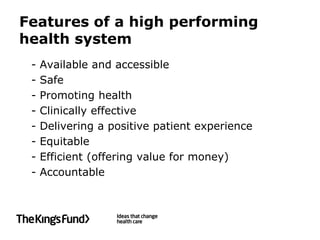
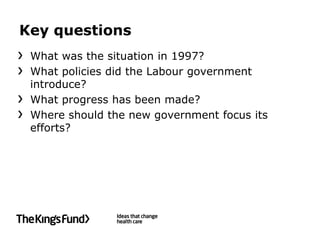
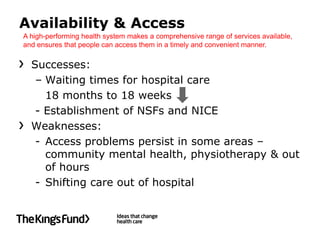
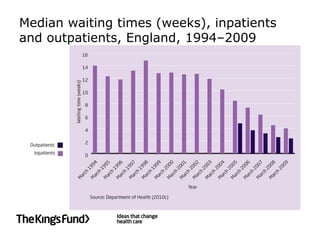
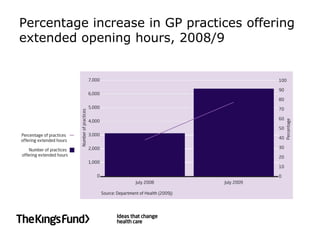
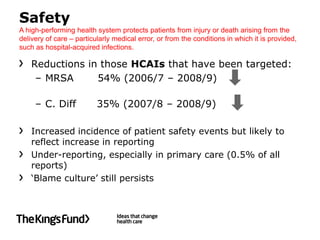
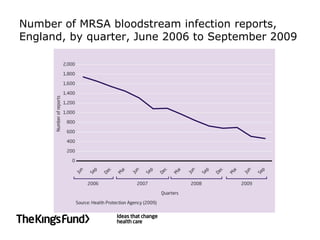
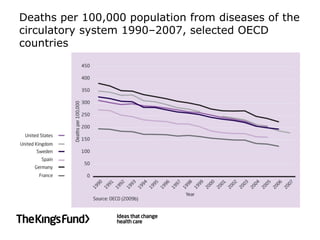
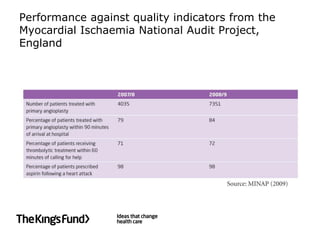
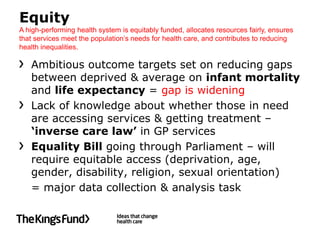
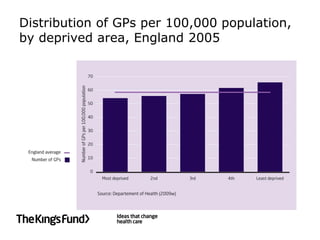
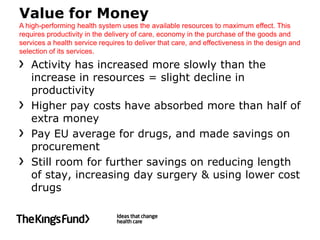
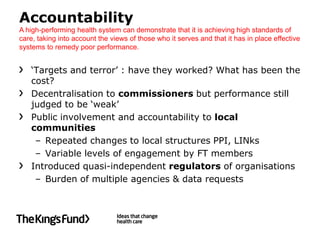
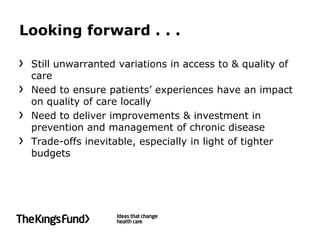
The document summarizes the progress of the NHS in England between 1997 and 2010 based on criteria for a high-performing health system. Key successes included reducing waiting times, establishing clinical standards, and improved health outcomes for major diseases. However, challenges remained around access to services, health inequalities, patient experience in mental health, and demonstrating value for money. Moving forward, ensuring consistent quality and addressing long-term conditions would be priorities in light of tighter budgets.