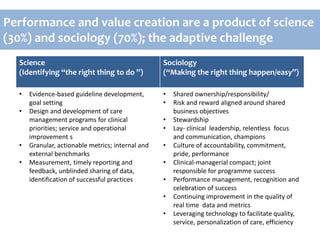
The document outlines a journey towards transforming the NHS into a community-based integrated health and care system, focusing on accountability, resource allocation, and patient empowerment. It emphasizes the importance of data-driven approaches and collaboration among healthcare providers to improve clinical outcomes and manage long-term conditions effectively. The strategy includes financial restructuring, the establishment of new governance models, and enhancing general practice contributions to create sustainable solutions for the population's health needs.
![• Integrated health and care system
• Accountability for clinical outcomes
• Align budgetary accountability with clinical decision to
commit resource
• Reduce / eliminate funding gap [£140m] by 18/19
• Vire resource into preventing hospital admissions and
reduce length of stay
• Support personal lifestyle behaviour change - reducing
prevalence/ burden of long term conditions
• Empower patients and carers to self-manage long term
conditions, support independent living
• Redirecting activity from secondary care into capable, at
scale primary care
Focus of Principia New Care Model transformation](https://image.slidesharecdn.com/stephenshortt-160311153106/85/Transforming-the-NHS-Stephen-Shortt-2-320.jpg)
![“Only physicians and provider organizations can put in place the set of
interdependent steps needed to improve value [the relationship between
outcomes and costs] , because ultimately value is determined by how
medicine is practiced and care is delivered.”](https://image.slidesharecdn.com/stephenshortt-160311153106/85/Transforming-the-NHS-Stephen-Shortt-4-320.jpg)
![[Urgency, capacity and knowing where to start]
• Understanding and managing risk; value based contracting; payment models;
transitioning to capitation
• Advanced data management capabilities ; use of actionable intelligence
• Re-imagining care model; care management processes; risk stratification
• Establishing preferred relationships with motivated and efficient specialists, partners
• Implement standardised care management protocols; tracking and managing
clinician behaviours and performance
• Technology and infrastructure requirements; EHR
• Reward systems , payment mechanisms aligned with organizational and system goals
to reward desired behaviours, cost utilization, quality and patient experience
• Activation of patients and families in managing own health and self determination
• Cross-system engagement, leadership and governance
• Implementing change in complex care organisations and networks
• Capital; financial protection
Technical challenges](https://image.slidesharecdn.com/stephenshortt-160311153106/85/Transforming-the-NHS-Stephen-Shortt-6-320.jpg)
![• Self assessment: insufficient capacity and capability to address systemic
issues of quality and financial sustainability as urgently as required, or
competencies required by a population health risk bearing organisation
• Proposal to recruit transformation partner/system integrator
• Harness efficiencies and expertise in long term relationship to :
• Modernise and create a fit for purpose care infrastructure
• Improve efficiency and quality of delivery
• Secure appropriate risk transfer to stimulate innovation and
performance management
• [Introduce capital] without increasing public sector debt
• Share accountability and risk for cost control and performance
• Actuarial feasibility analysis (14 organisations inc. primary care and LAs)
• Programme design and partnership development
14
Developing a fit for purpose accountable care system](https://image.slidesharecdn.com/stephenshortt-160311153106/85/Transforming-the-NHS-Stephen-Shortt-14-320.jpg)