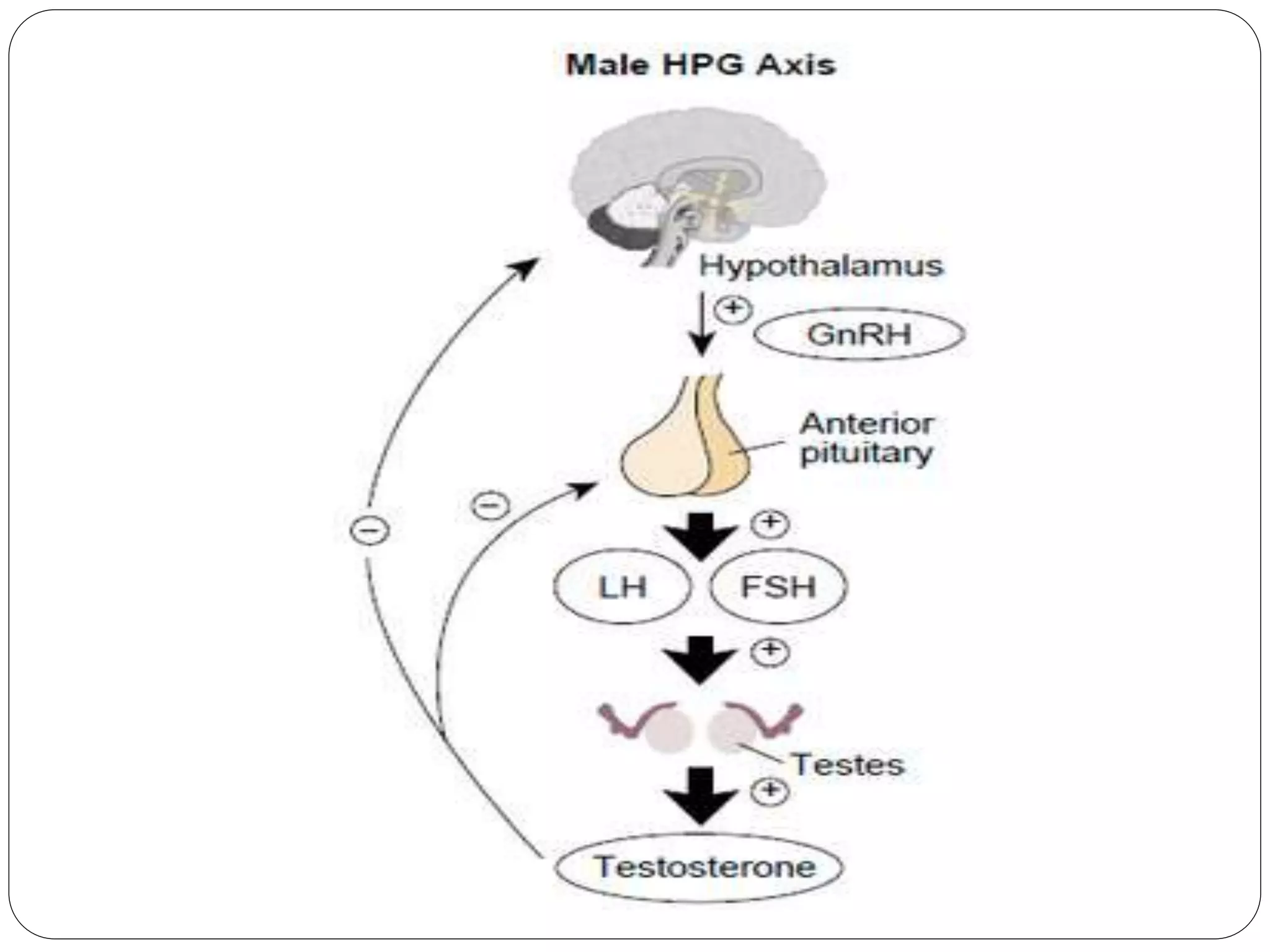
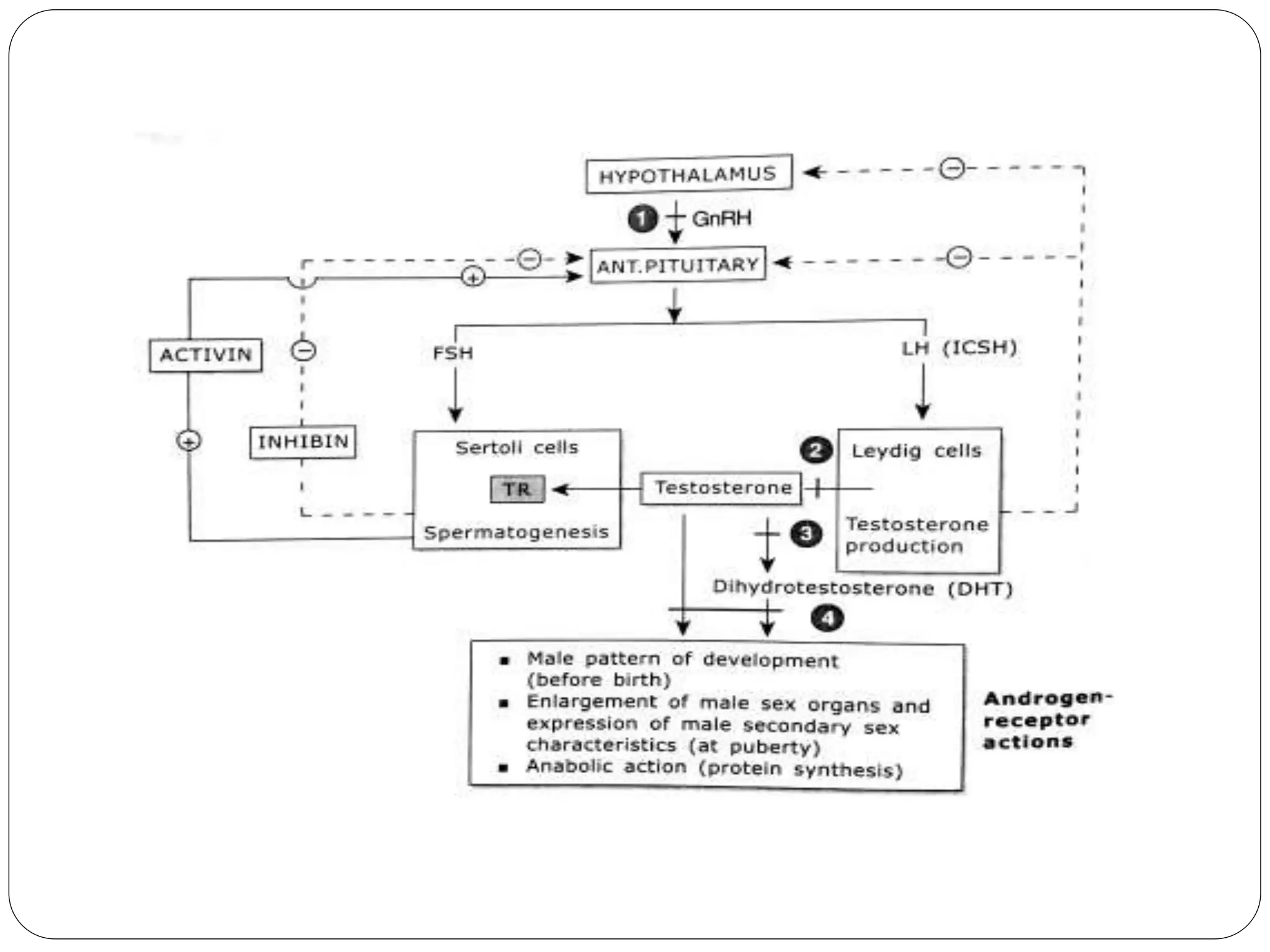
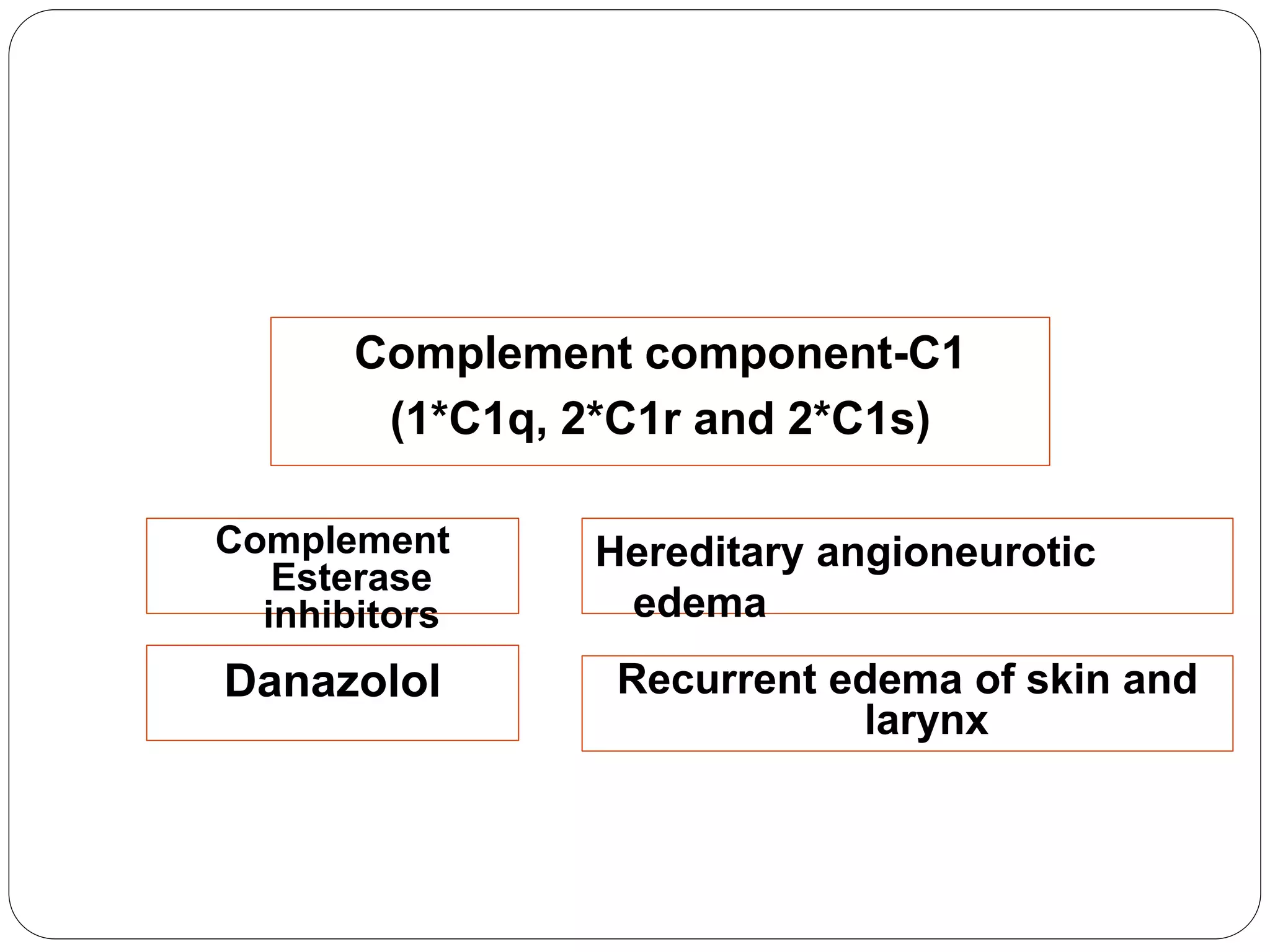
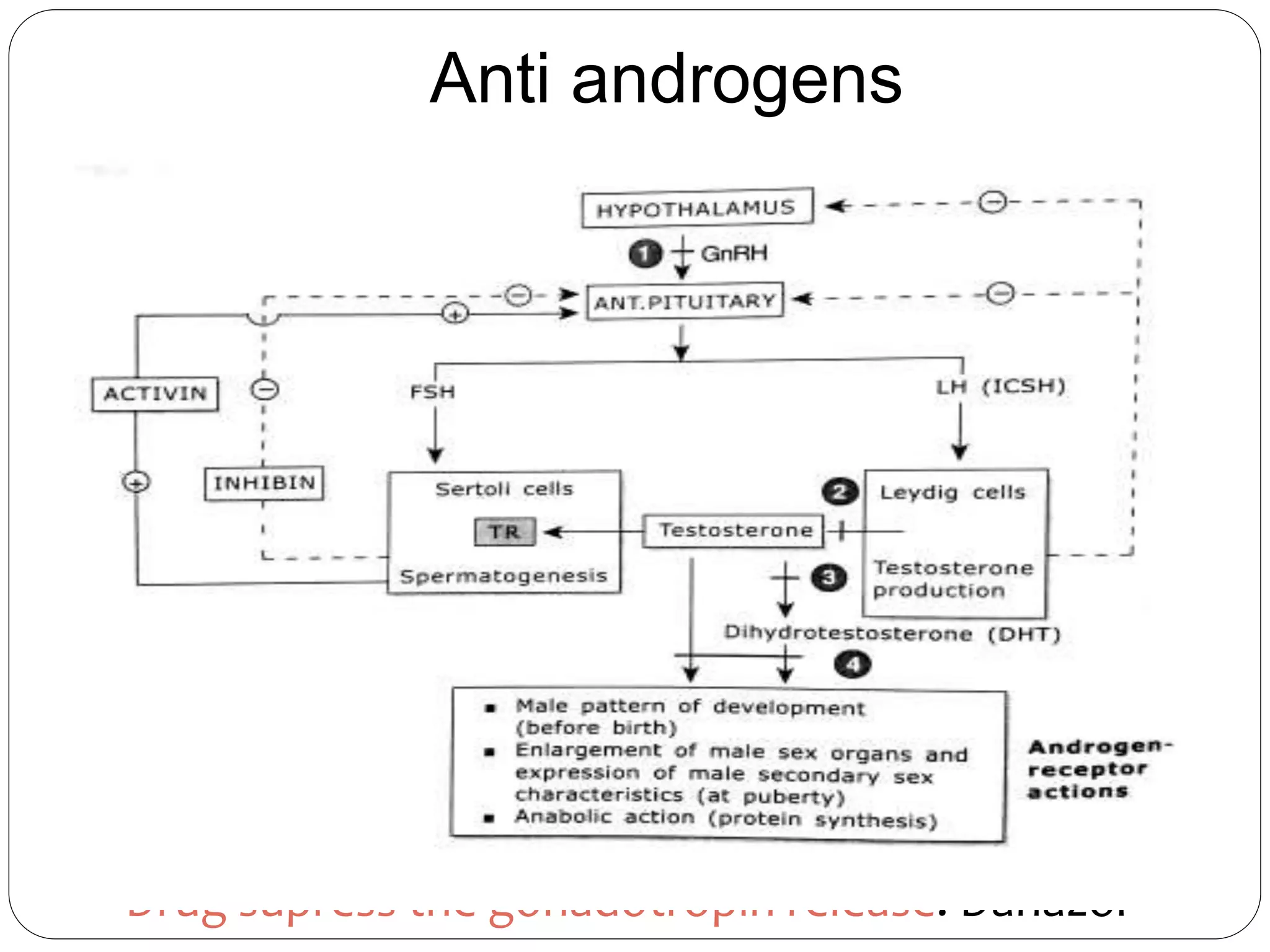
This document discusses androgens, anabolic steroids, and treatments for erectile dysfunction. It describes how androgens such as testosterone are naturally produced and have effects on sexual development, muscle growth, and behavior. Anabolic steroids are synthetic derivatives of testosterone that are sometimes abused for their muscle building effects. The document outlines the mechanisms, effects, and side effects of various androgens and anabolic steroids. It also discusses treatments for lowering androgen levels including anti-androgens and 5-alpha reductase inhibitors. Finally, it summarizes common pharmaceutical treatments for erectile dysfunction including phosphodiesterase-5 inhibitors and alprostadil injections.