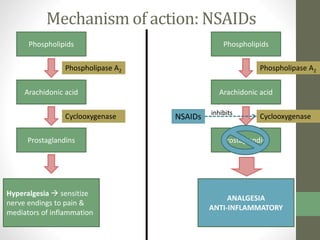
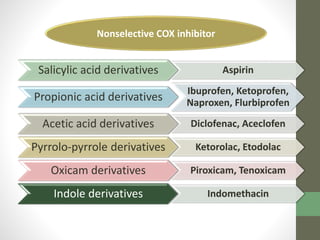
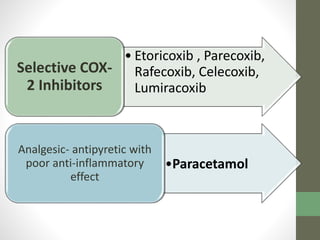
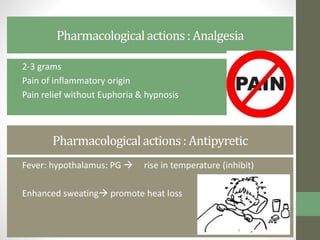
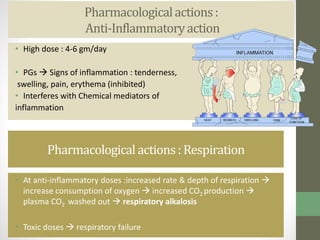
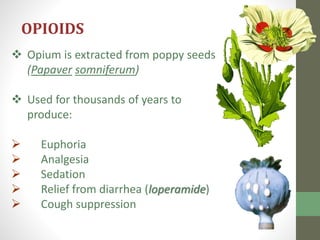
1. The document discusses various classes of analgesics including centrally acting analgesics like opioids and peripherally acting analgesics like non-steroidal anti-inflammatory drugs (NSAIDs).
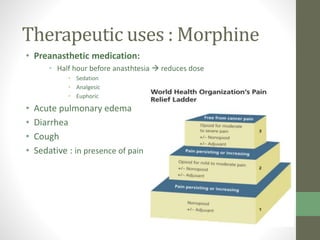
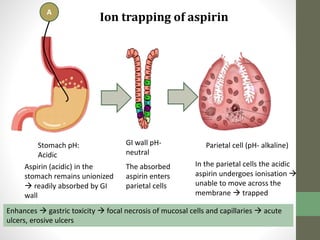
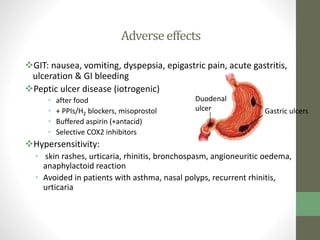
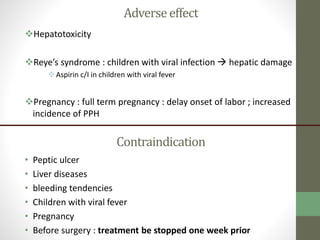
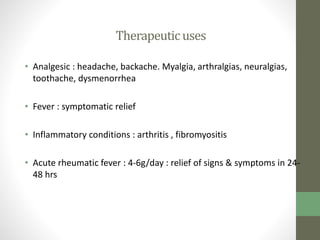
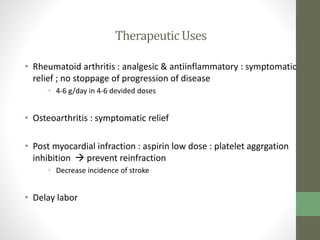
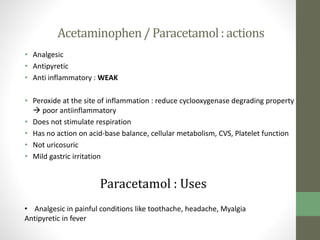
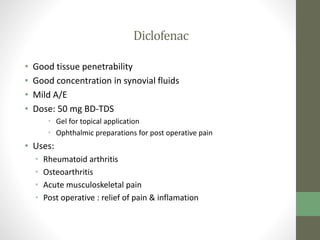
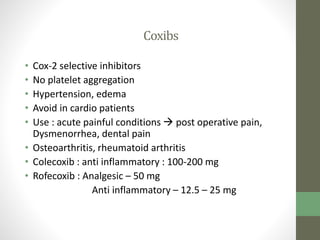
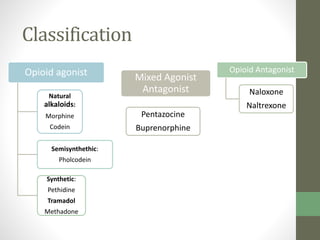
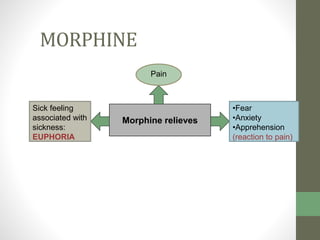
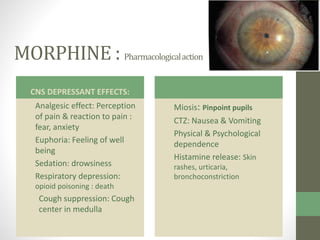
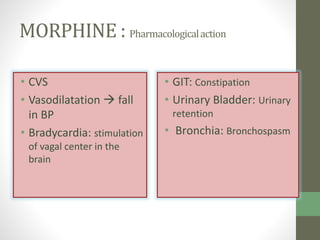
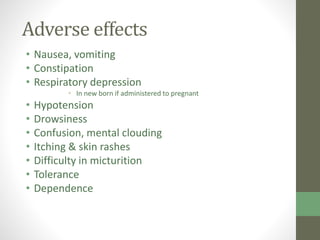
2. It specifically describes the properties and uses of morphine, aspirin, ibuprofen, piroxicam, and paracetamol. Morphine is an opioid analgesic that provides pain relief and euphoria but can cause respiratory depression and dependence. Aspirin is an NSAID that reduces fever and inflammation while also inhibiting platelet aggregation.
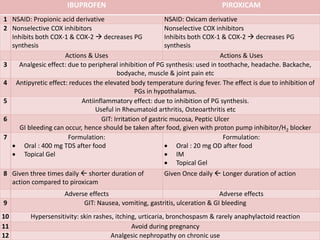
3. Ibuprofen, piroxicam, and paracetamol are NSAIDs as well but differ in their duration of action, formulations, and



![Therapeutic uses : Morphine
• ANALGESIC:
• Acut myocardial infarction
• Burns
• Pulmonary embolism
• Fracture of mandible and long bones
• Bullet wounds
• Renal & biliary colic [ + atropine to control spasmogenic effect of
morphine]
• Terminal stage of cancer](https://image.slidesharecdn.com/analgesicsopoidsnsaidsunitynursingshare-210809133907/85/Analgesics-opoids-NSAIDs-nursing-10-320.jpg)