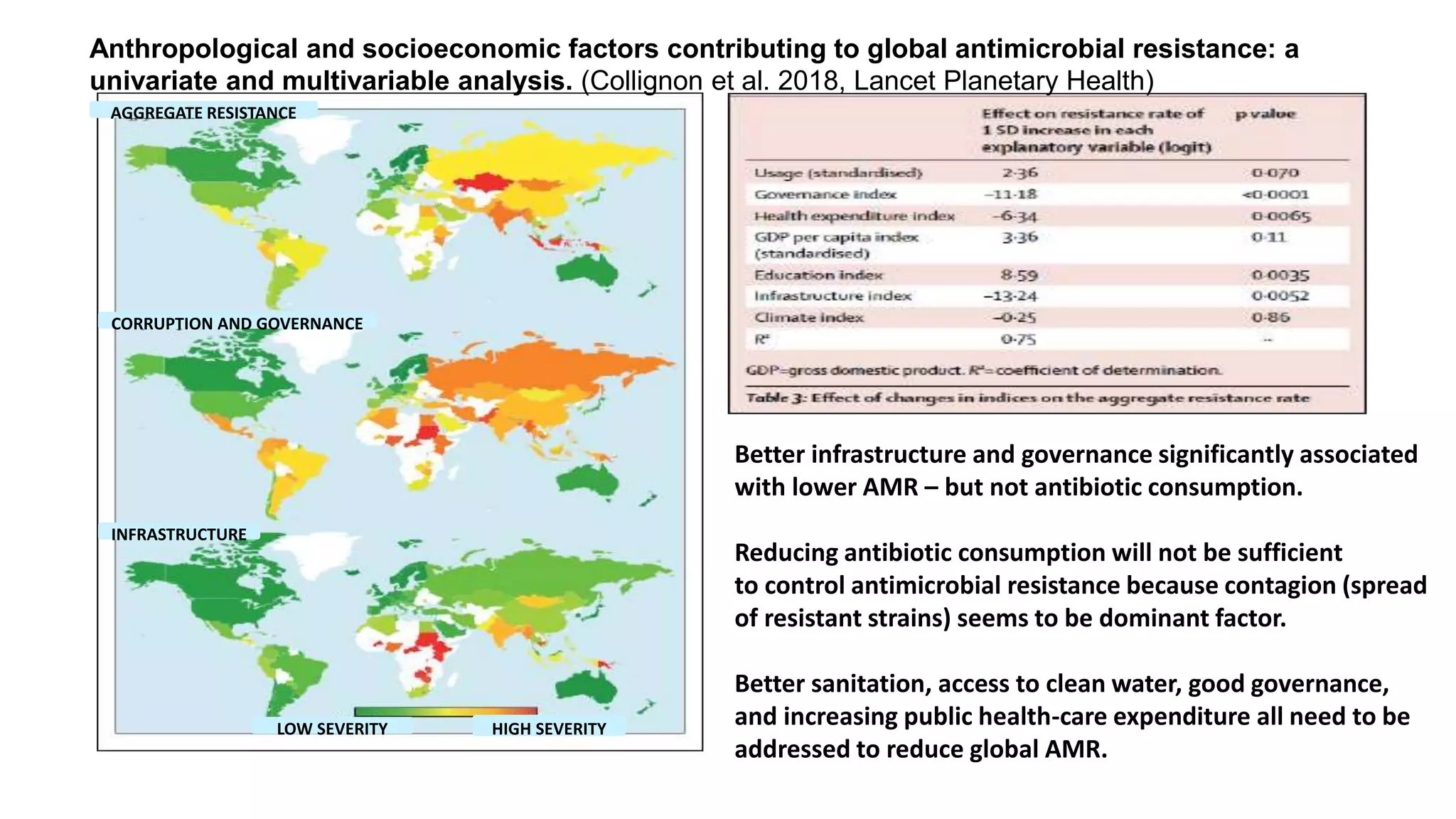
The document discusses the global challenge of antimicrobial resistance (AMR), framing it as not just a public health issue but a developmental challenge, particularly for low- and middle-income countries. It emphasizes the need for a multifaceted approach that addresses behavioral, social, and economic factors, rather than solely focusing on reducing antimicrobial consumption. Key recommendations include strengthening public health systems and implementing adaptive strategies informed by context-specific research to effectively combat AMR.





![Seeking to articulate the importance of context in relation to AMR
9
Recognizing the importance of context and
the distinction between emergence and
spread
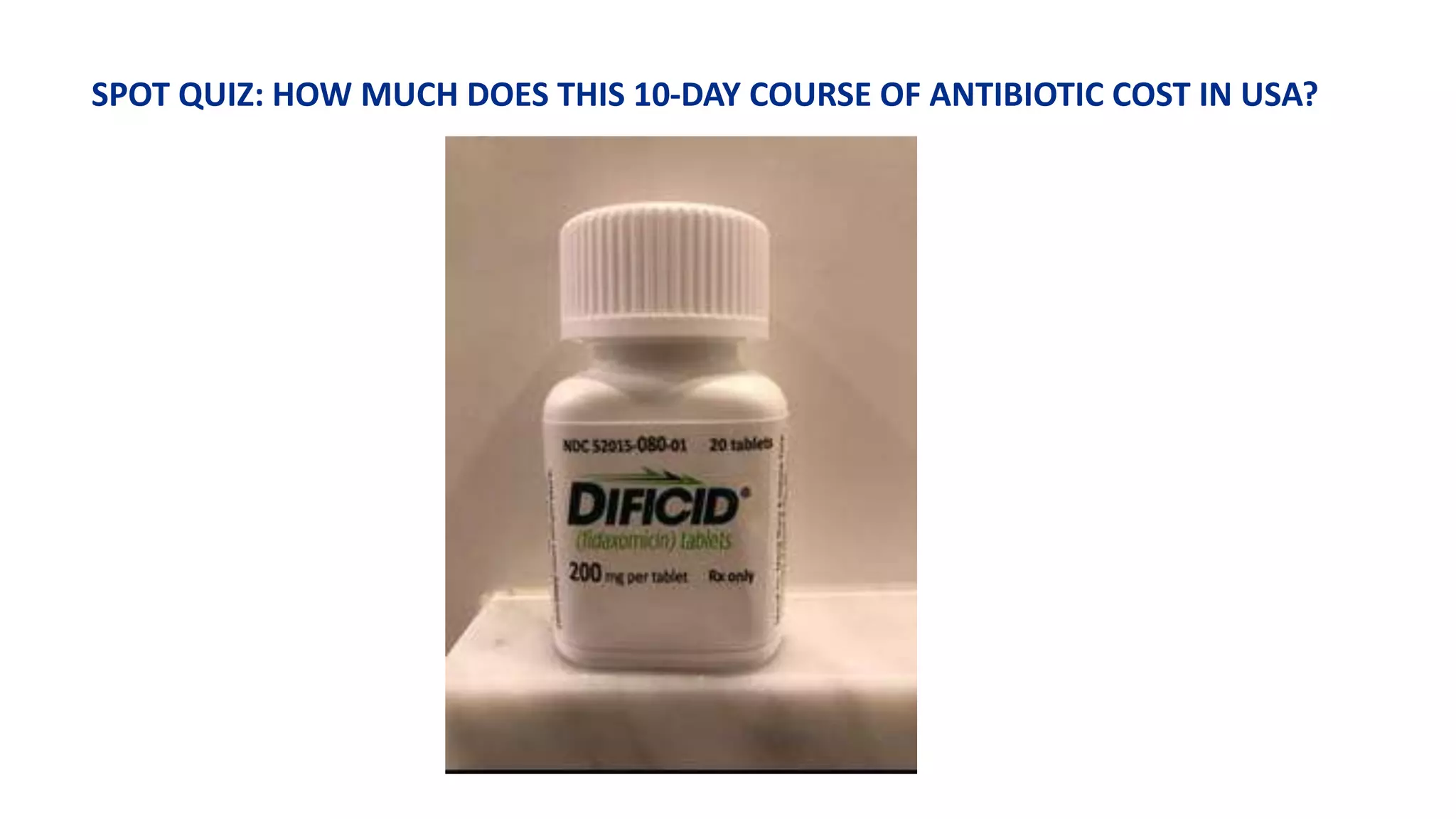
• AMR is often understood in terms of use [mis- and over-
use] of antimicrobials; however, limiting consumption of
antimicrobials will not be sufficient to control AMR.
• Context, determined by anthropological and
socioeconomic factors, is critical to understanding the
spread of resistance determinants.
• The use of antimicrobials has a bearing on emergence
of AMR, but the spread -sometimes referred to as
contagion- is driven by context.
• We need to address the underlying weaknesses of
systems to be able to address AMR; hence the need for
alignment of the AMR and Sustainable Development
agendas.
• AMR specific plus AMR sensitive investments.](https://image.slidesharecdn.com/amrjonathan-190308083314/75/Pulling-together-to-beat-superbugs-9-2048.jpg)



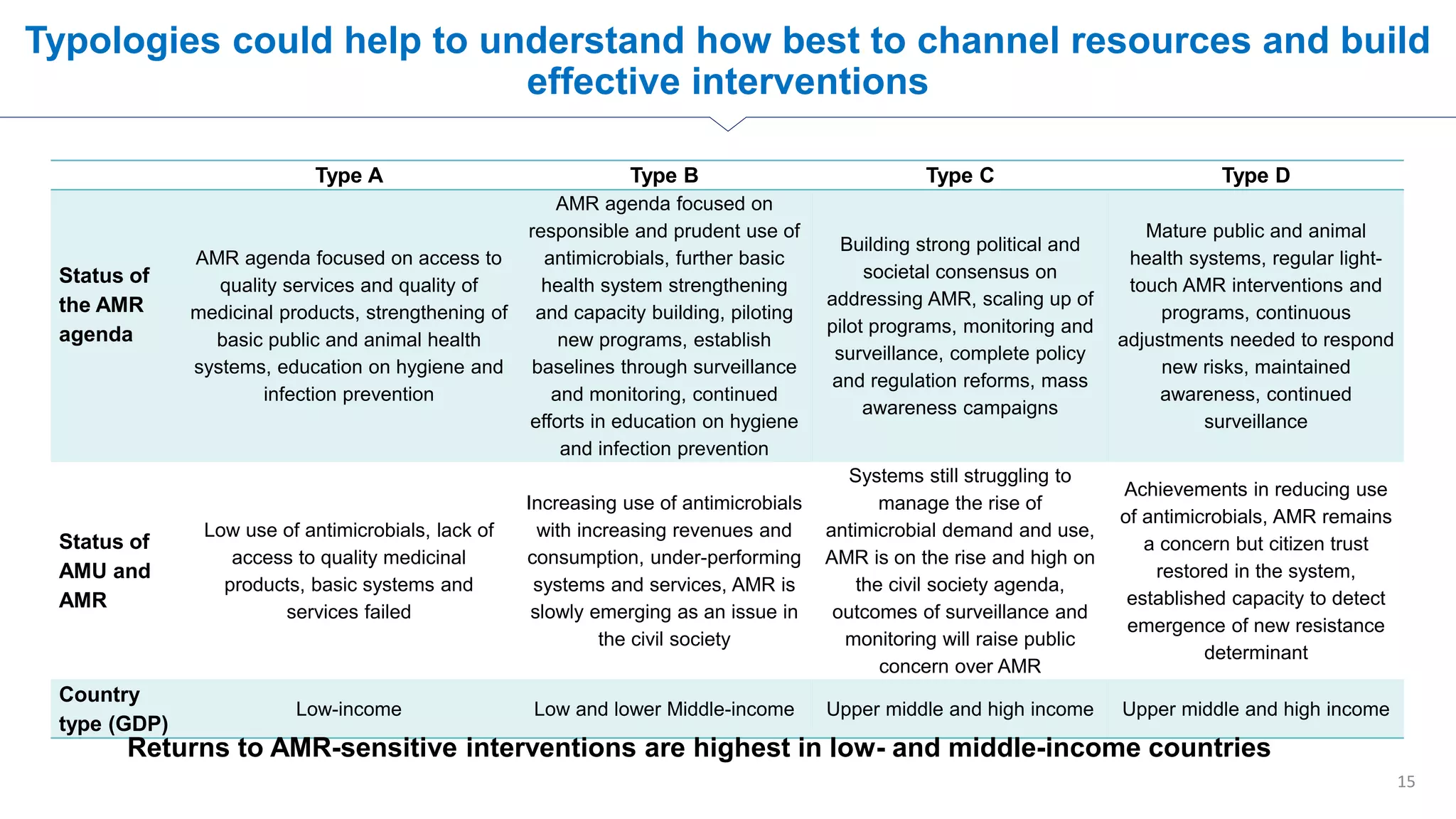
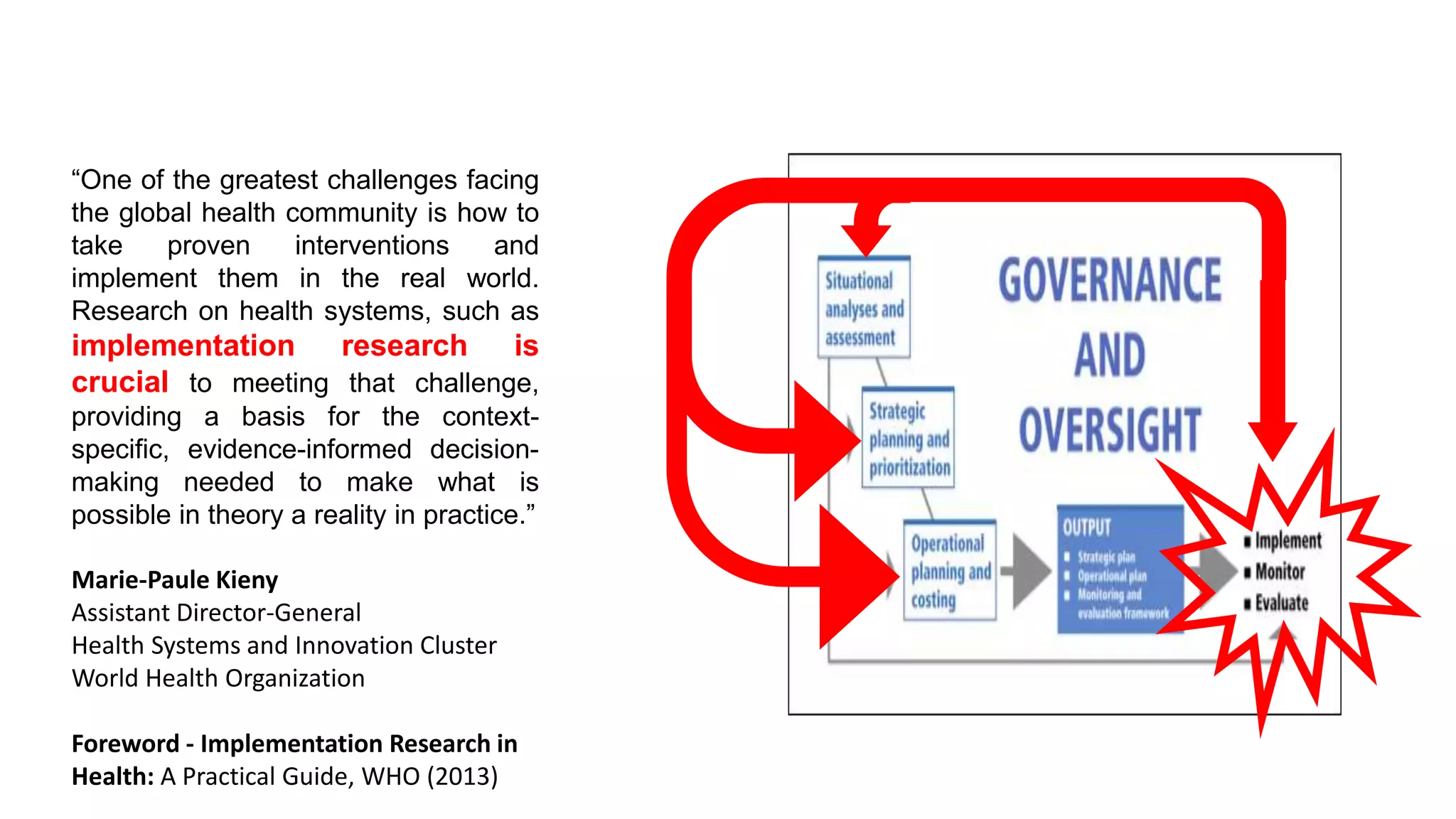
![Describing typologies of countries, in terms of AMR risk
14
Type A Type B Type C Type D
Level of
economic
development
Low
income
Low & lower-
middle income
Upper-middle
& high income
Upper-middle
& high income
Antimicrobial
use
Low High High Low
Exposure to
other
contextual
risk factors
High High Medium Low
Expected level
of AMR
Medium High Medium/High Low
Lower- and Middle-income countries have the most dangerous
combination of risk factors for emergence and spread of
antimicrobial resistance
While the theoretical curve [above] exposes a historical transition process for countries from type A to D, the global action on AMR is expected to
offer avenues for new trajectories towards type D.
Type A Type B Type C Type D](https://image.slidesharecdn.com/amrjonathan-190308083314/75/Pulling-together-to-beat-superbugs-14-2048.jpg)