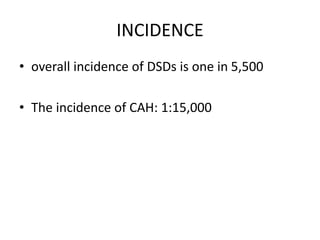
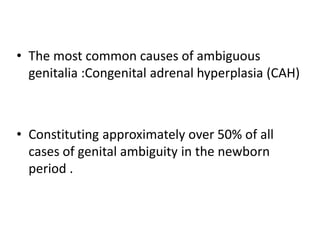
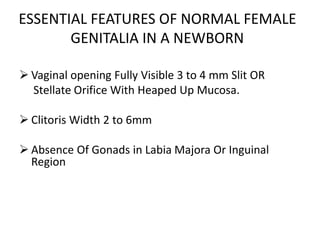
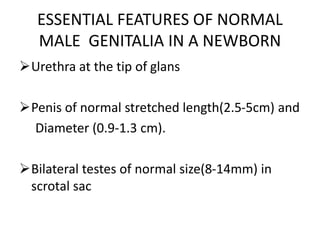
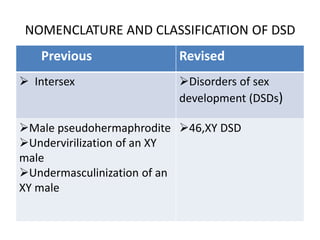
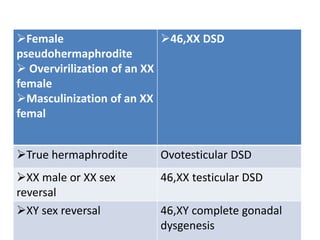
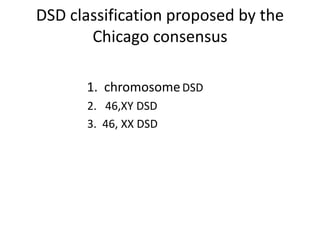
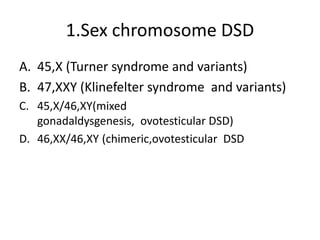
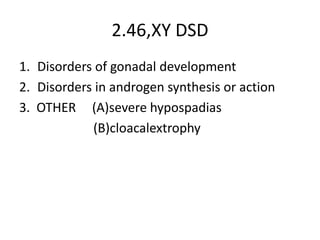
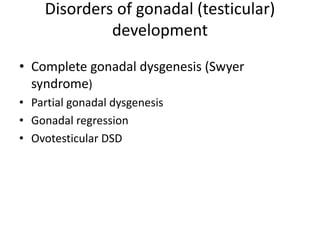
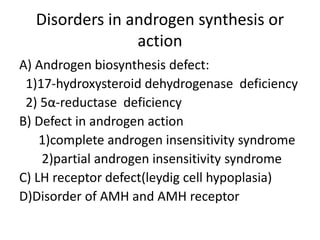
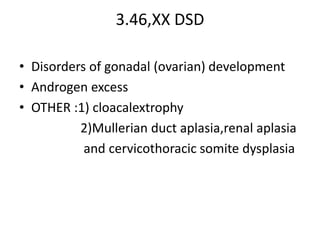
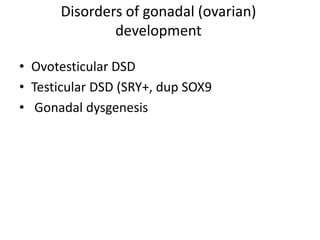
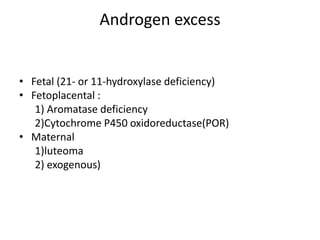
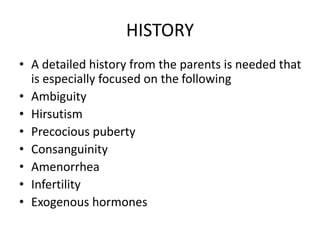
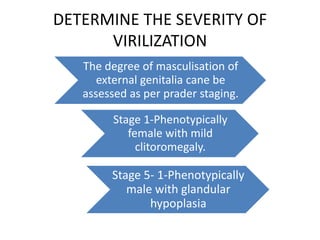
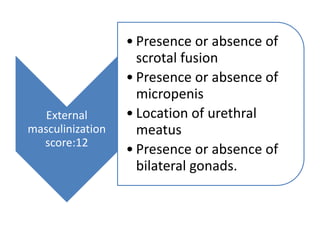
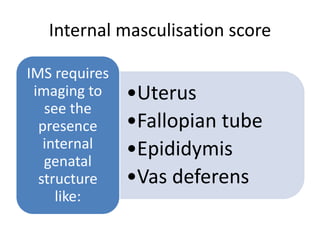
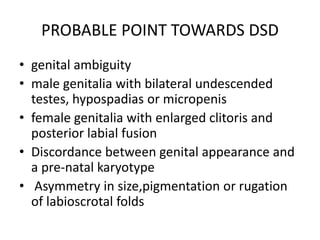
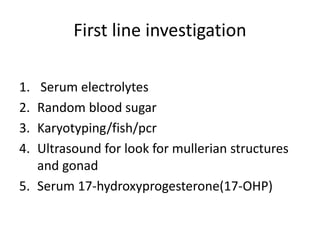
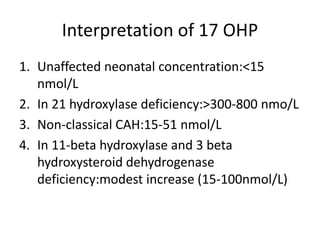
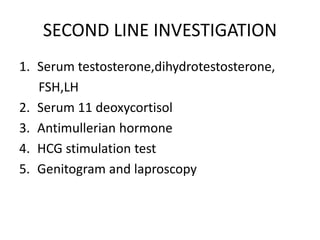
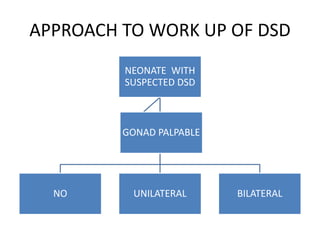
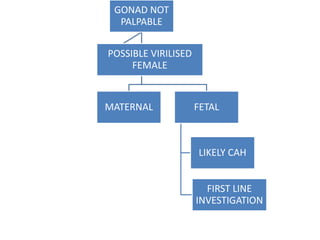
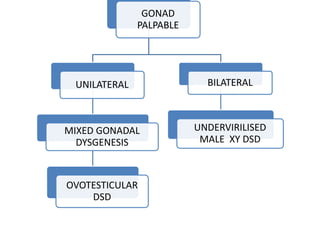
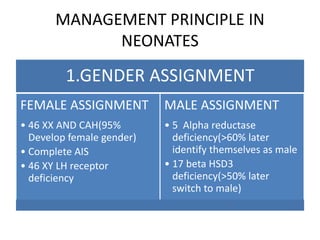
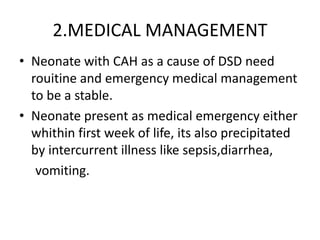
The document discusses the approach to disorders of sex differentiation (DSDs). It defines DSDs as congenital conditions associated with atypical development of chromosomal, gonadal, or anatomical sex. The evaluation and management of DSDs is complex and requires a multidisciplinary team approach. Initial assessment involves a detailed history, physical exam focusing on genital anatomy, and first-line lab investigations including karyotyping and hormones. Gender assignment and medical management are based on the underlying diagnosis and severity of virilization.