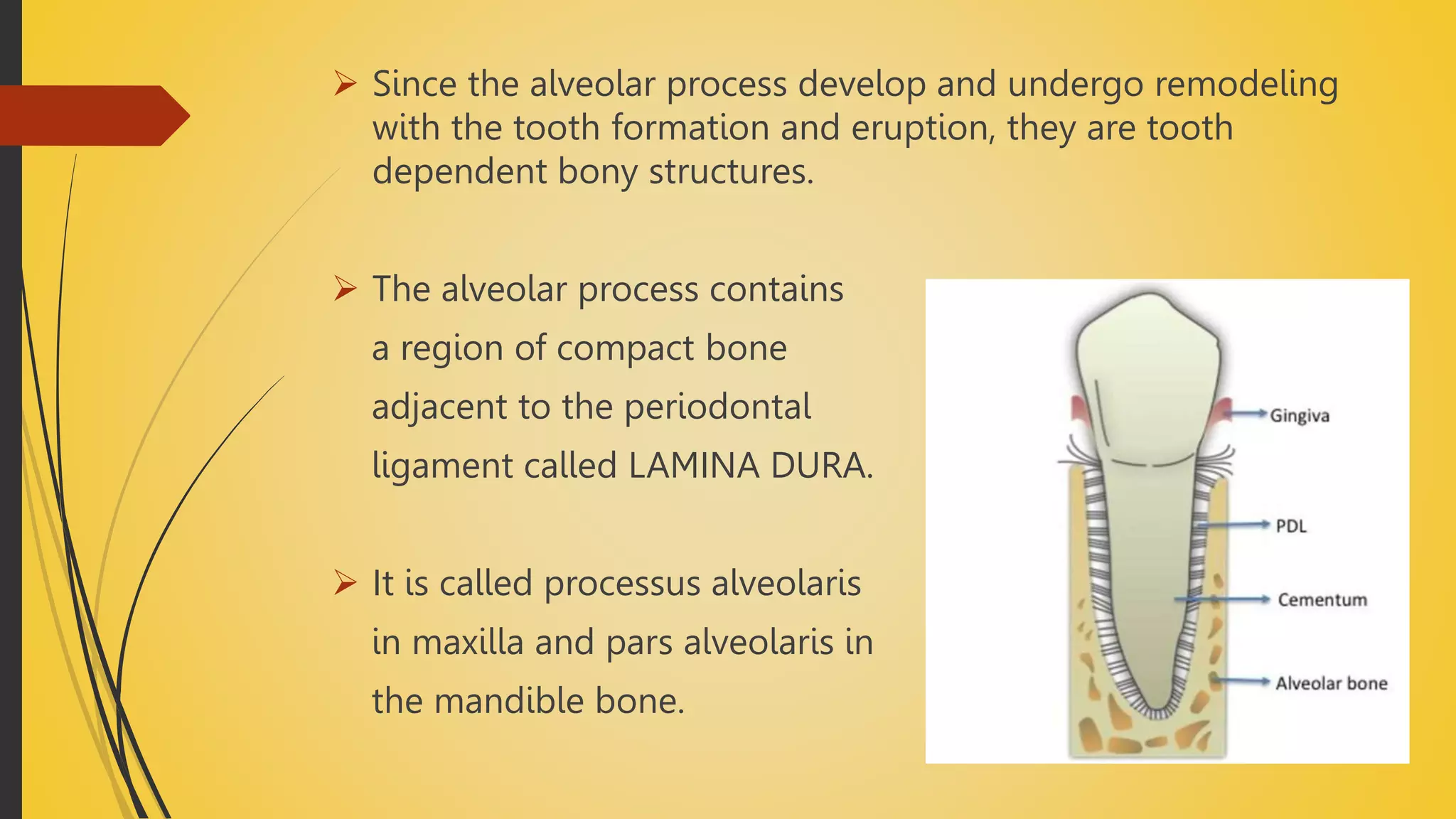
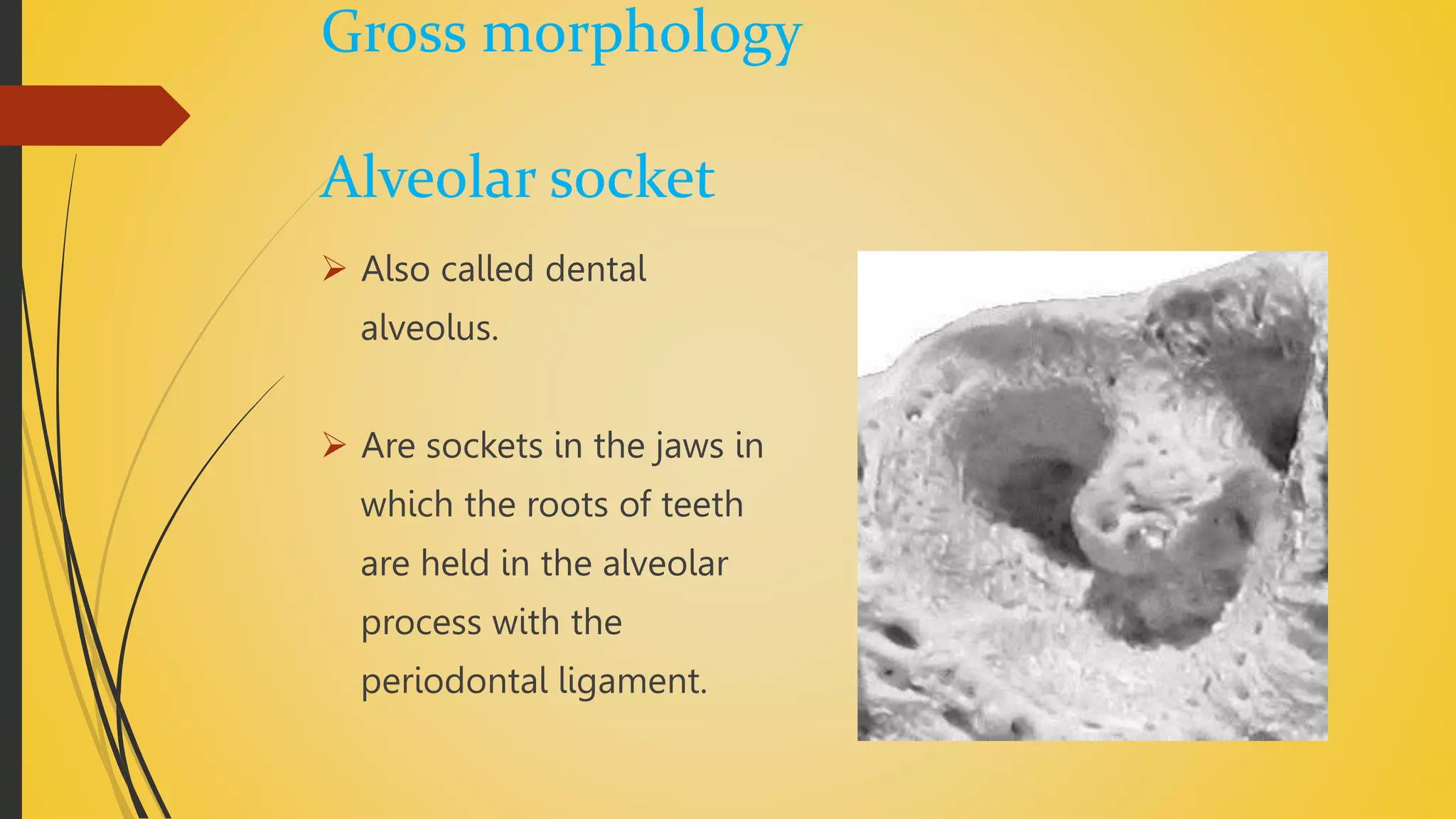
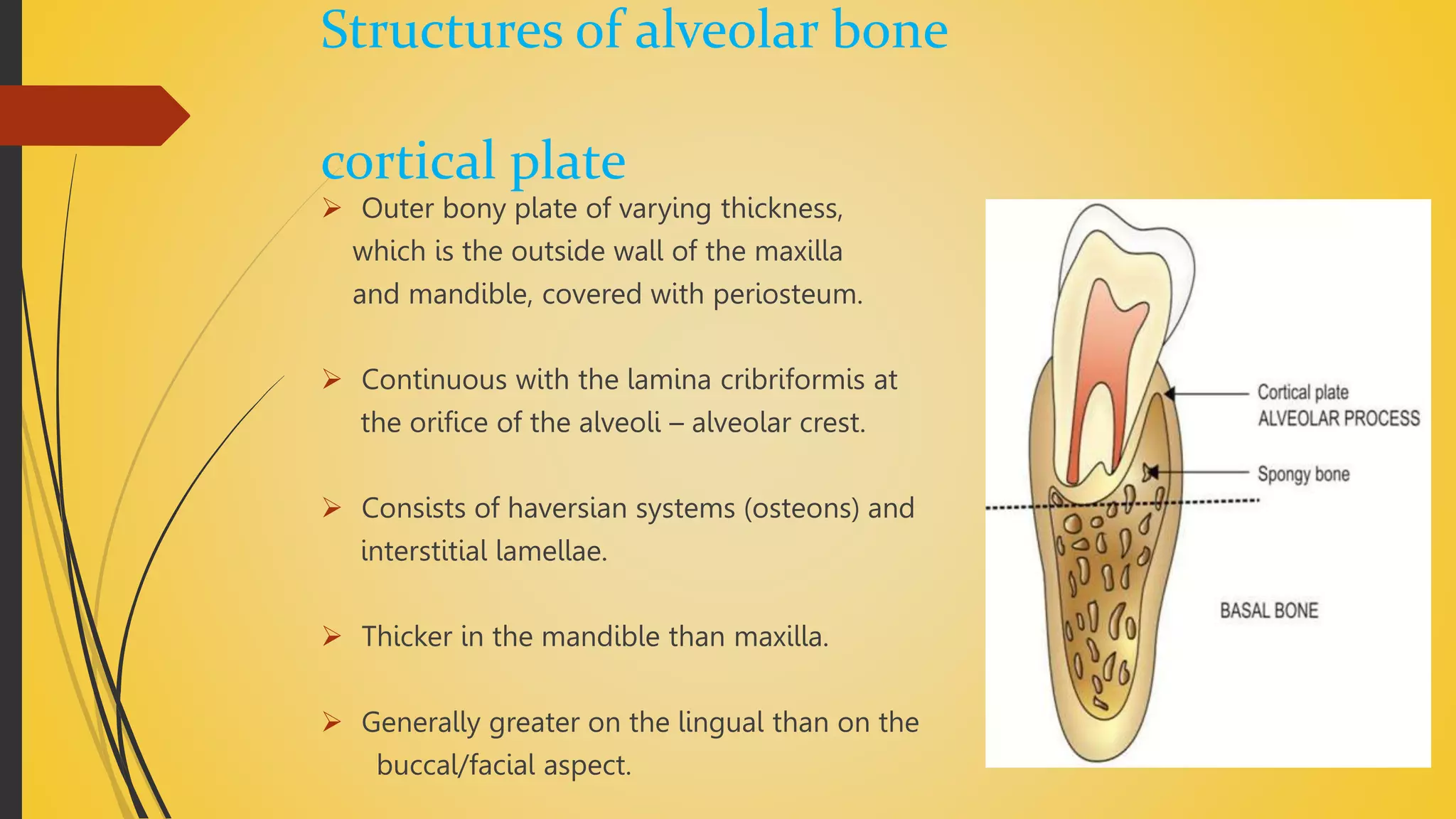
The document discusses the anatomy and structure of alveolar bone. It begins by defining alveolar bone as the portion of the maxilla and mandible that supports tooth roots. It then describes the functions of alveolar bone in supporting teeth and distributing occlusal forces. The document outlines the cellular components of bone, including osteoprogenitor cells, osteoblasts, osteocytes, and osteoclasts. It also discusses the vascular supply, Sharpey's fibers, and gross morphological features of alveolar bone, such as the alveolar socket and interdental septa.