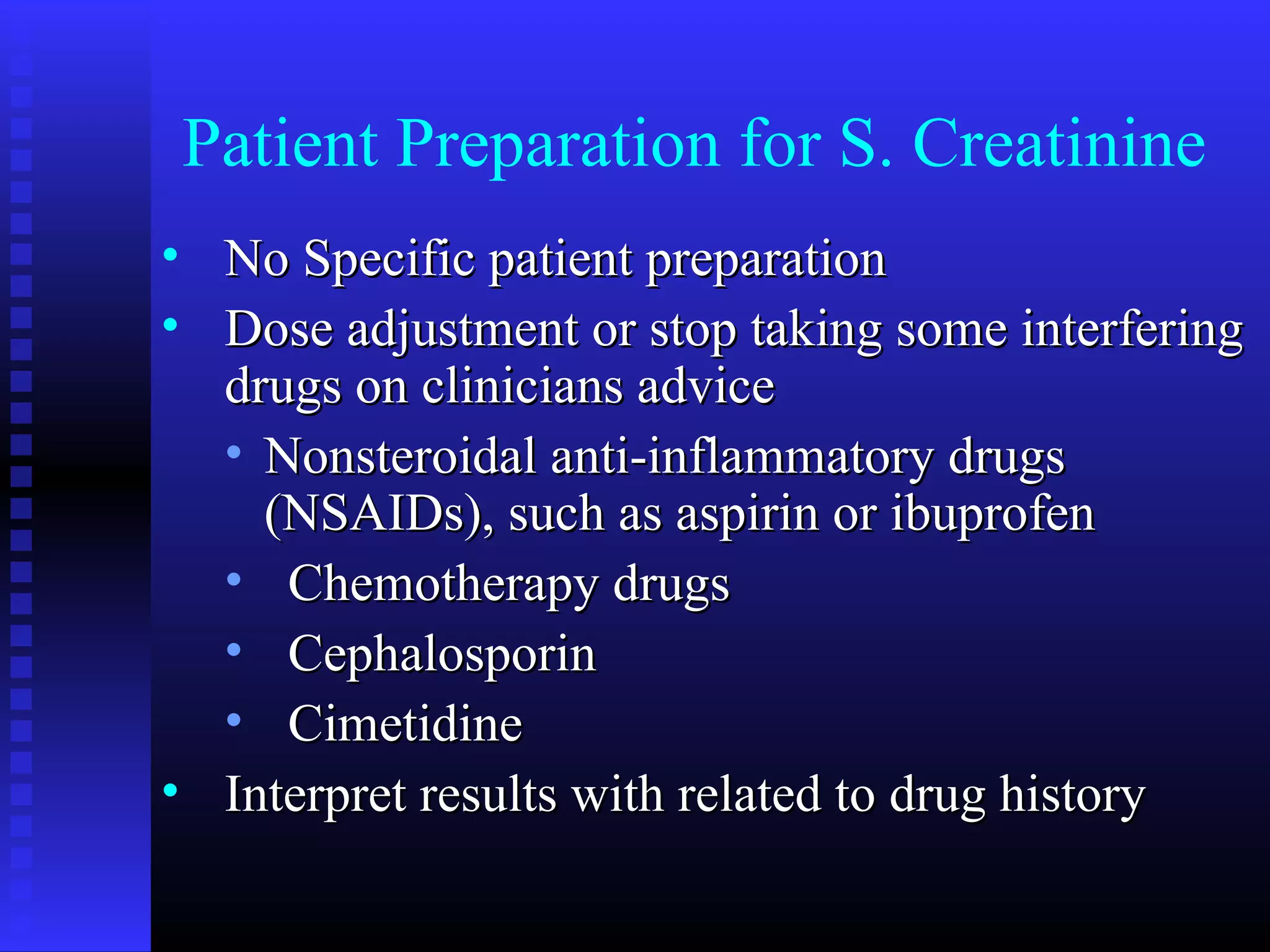
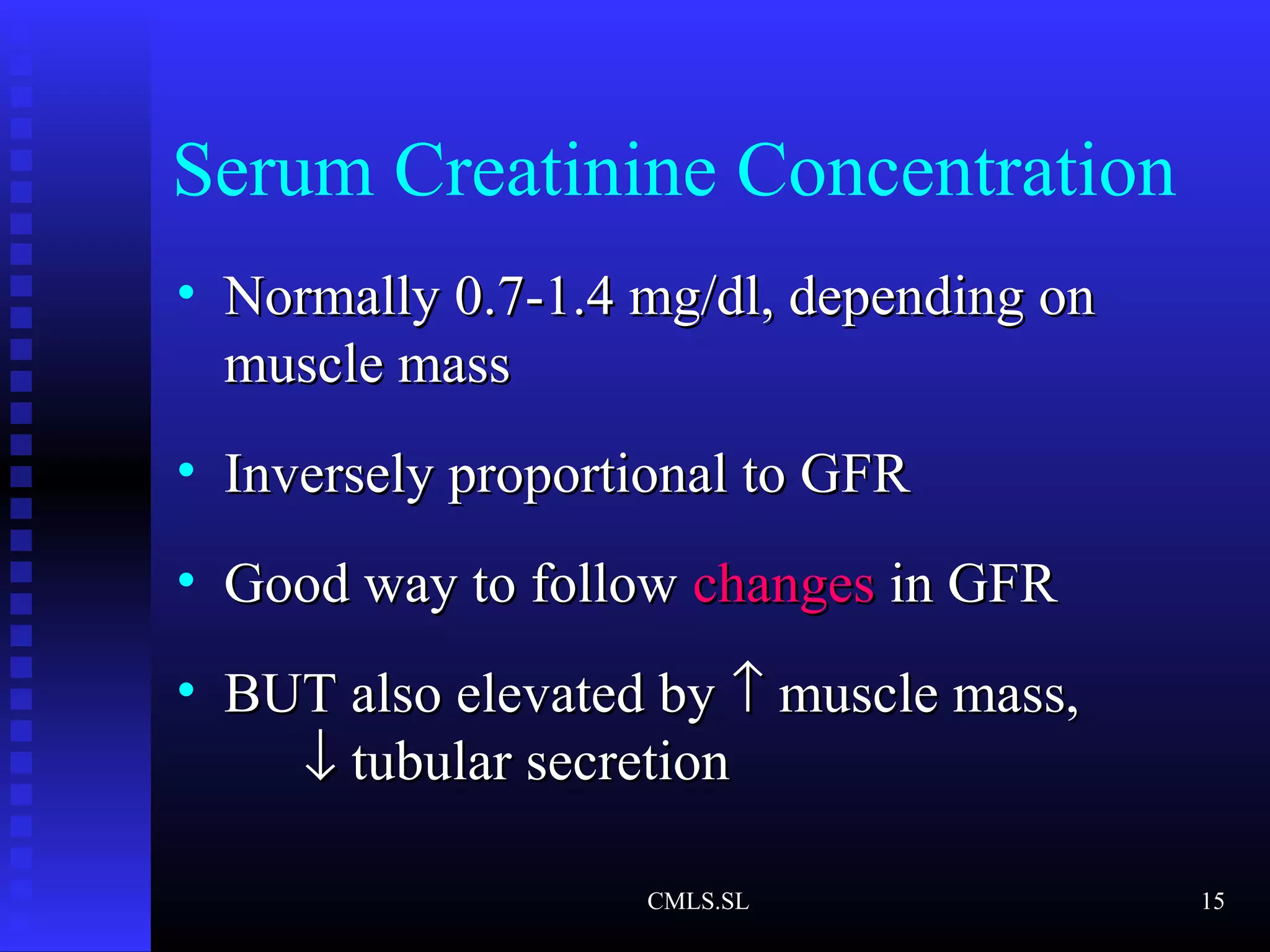
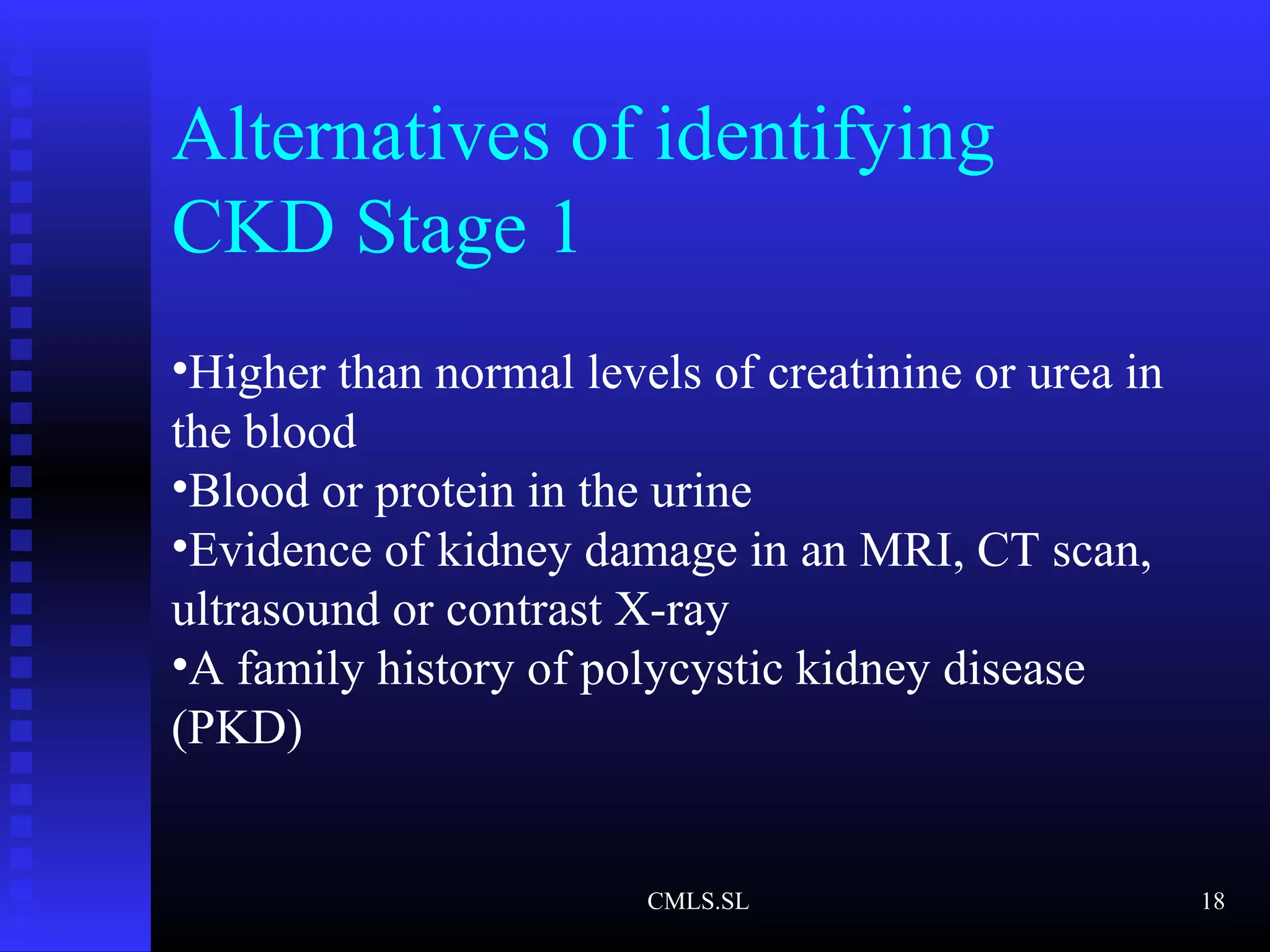
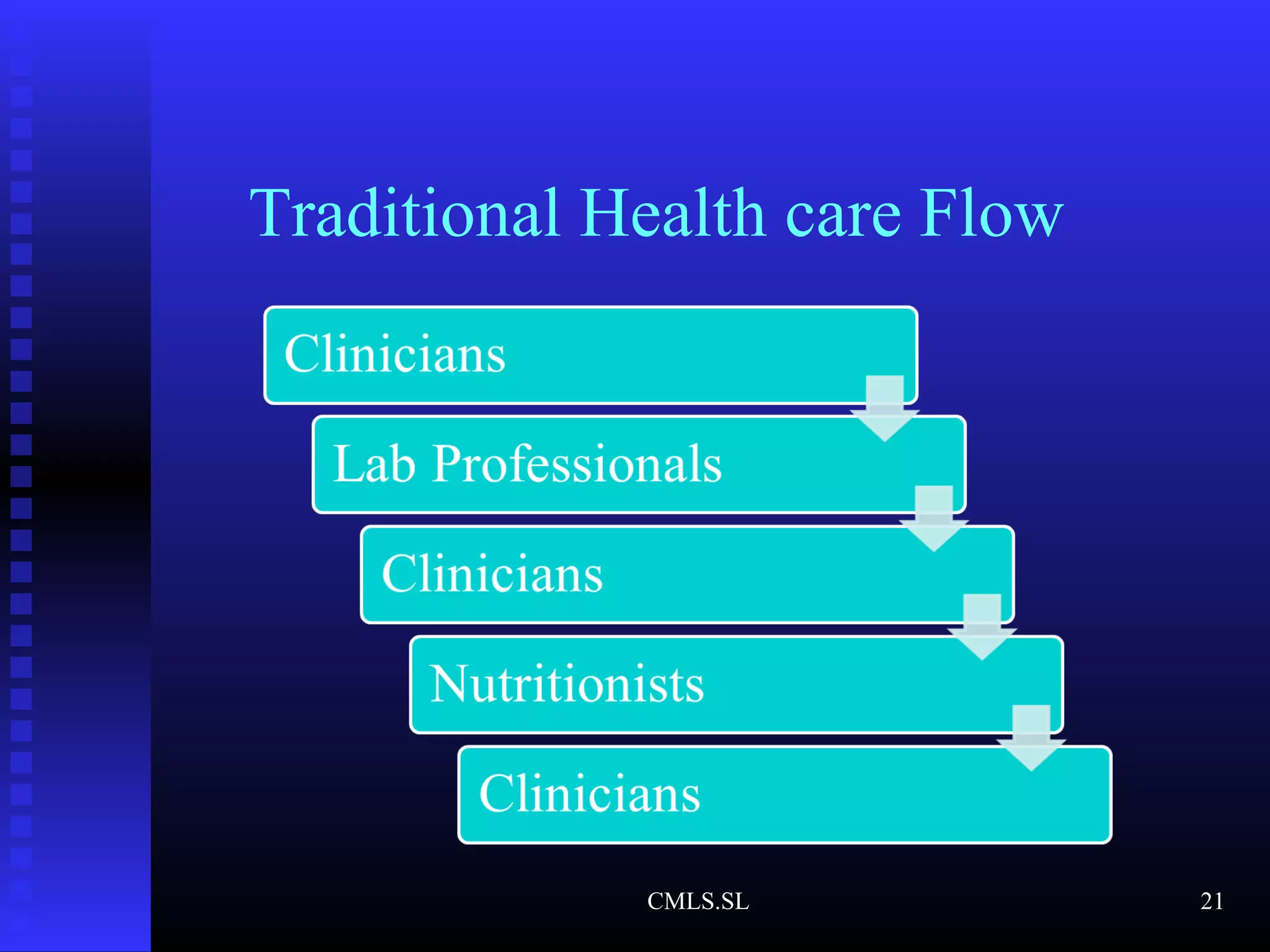
The document discusses the accuracy and management of laboratory parameters in chronic kidney disease (CKD), highlighting various risk factors, types of assays, and renal function tests. It emphasizes the importance of glomerular filtration rate (GFR) and serum creatinine in assessing kidney function, while also identifying potential interfering factors and patient preparation guidelines. Furthermore, it addresses alternative methods for identifying CKD stages and suggests future approaches for improving sensitivity in testing and patient-centered care.