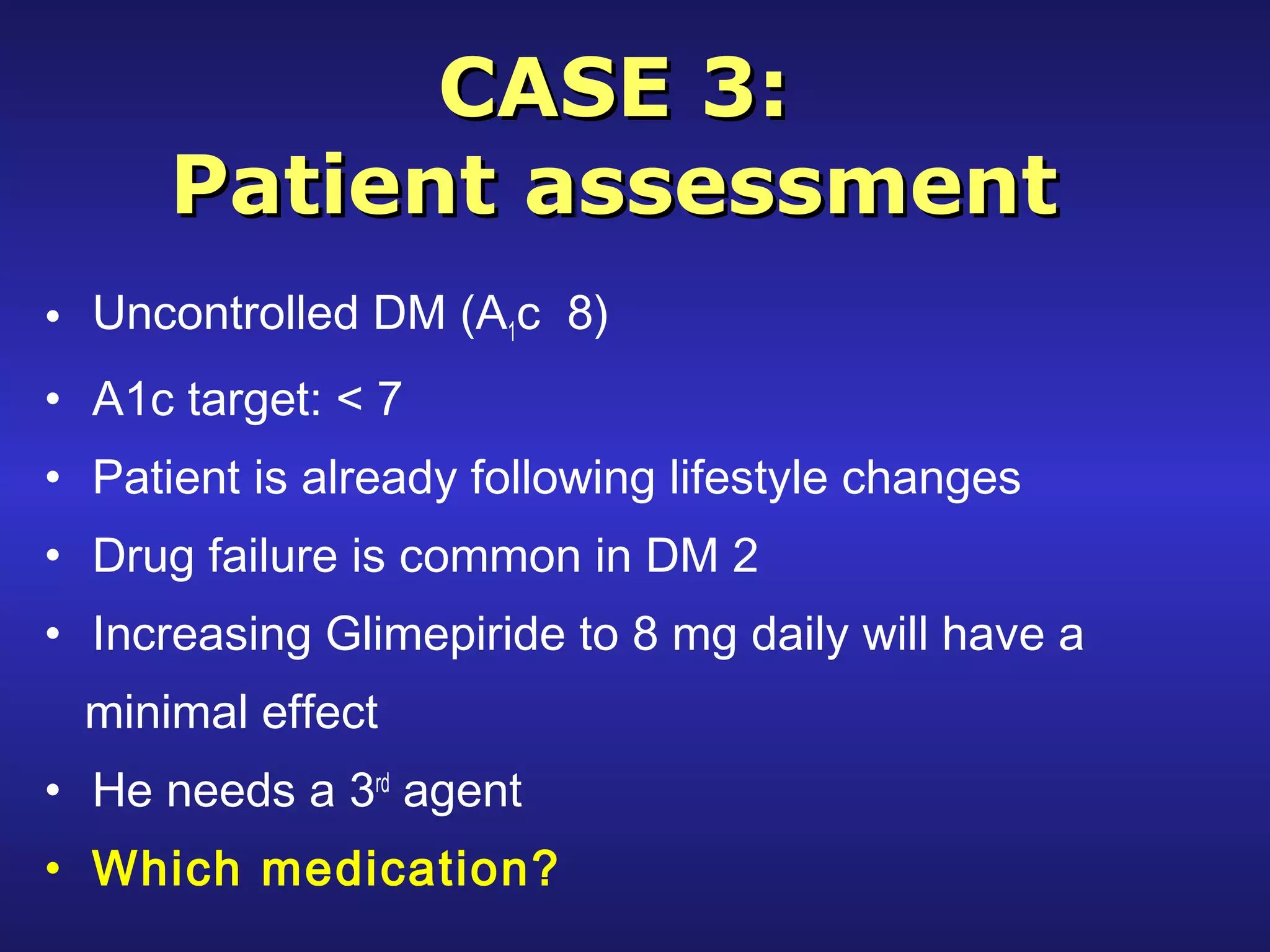
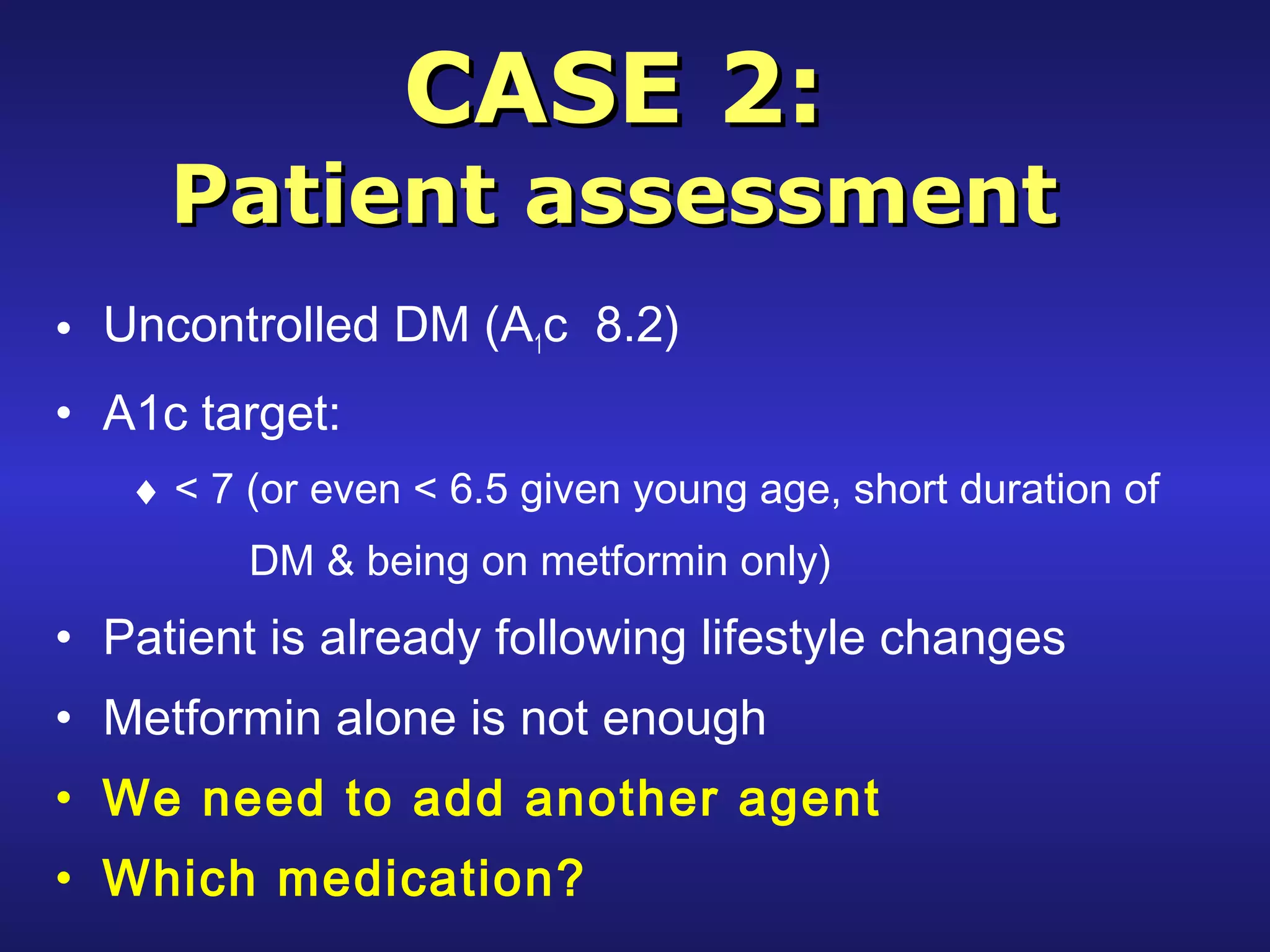
This document provides guidance on approaching and managing type 2 diabetes through non-insulin glucose-lowering therapy. It discusses evaluating patients, setting individualized A1C targets, implementing lifestyle changes, and initiating metformin as first-line treatment. If metformin alone does not control blood sugar, the document reviews additional options like sulfonylureas, DPP-4 inhibitors, GLP-1 receptor agonists, and SGLT2 inhibitors; comparing their mechanisms of action, dosing, side effects, and pros/cons. The overall approach emphasizes a treatment plan tailored to each patient's history, comorbidities, and goals of care.
























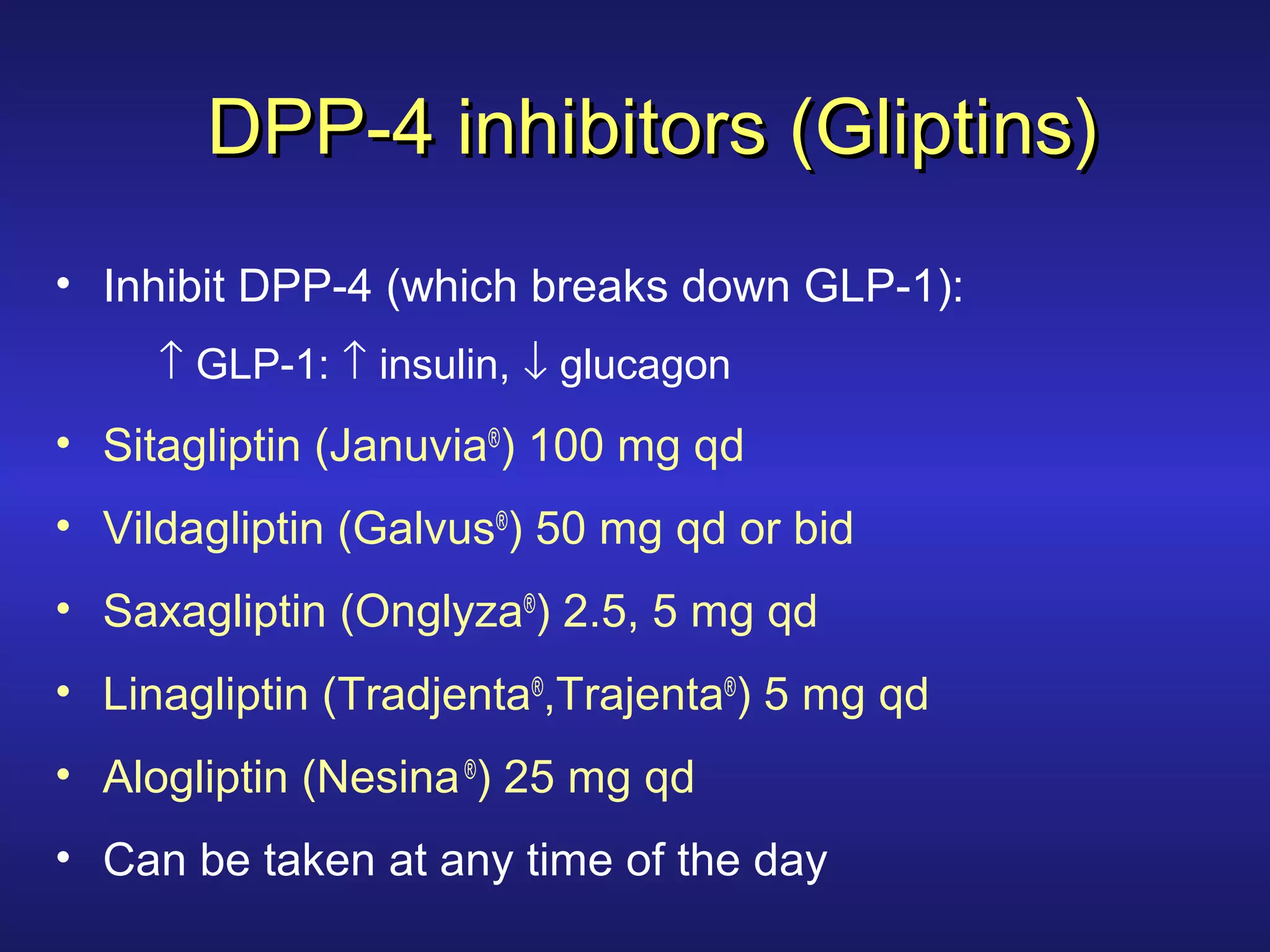




![GLP-1 RA examplesGLP-1 RA examples
Exenatide (Byetta®
)
• 5 micrograms bid (within 1 hour before main meals)
•Maximum dose: 10 micrograms bid
•Long-acting (Bydureon®
) [2 mg once/week]
Liraglutide (Victoza®
)
•Start 0.6 mg daily for 1-2 weeks then if tolerated increase to
1.2 mg qd
•Maximum dose: 1.8 mg qd
•Take at any time of the day](https://image.slidesharecdn.com/non-insulinglucose-loweringtherapy-p-190212181518/75/Non-insulin-glucose-lowering-therapy-in-type-2-DM-34-2048.jpg)