This document discusses ABO incompatibility between a mother and fetus/newborn. The main points covered are:
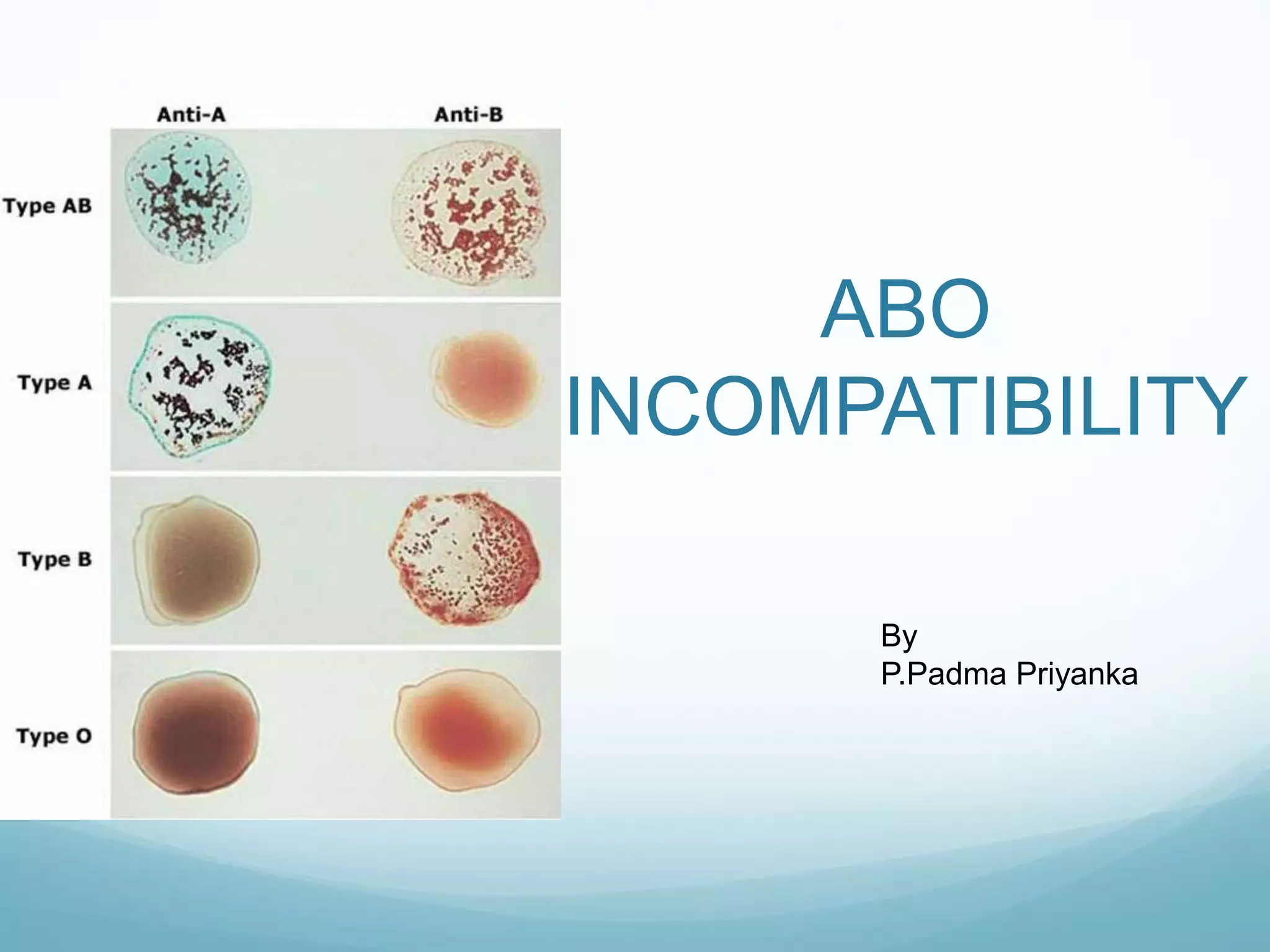
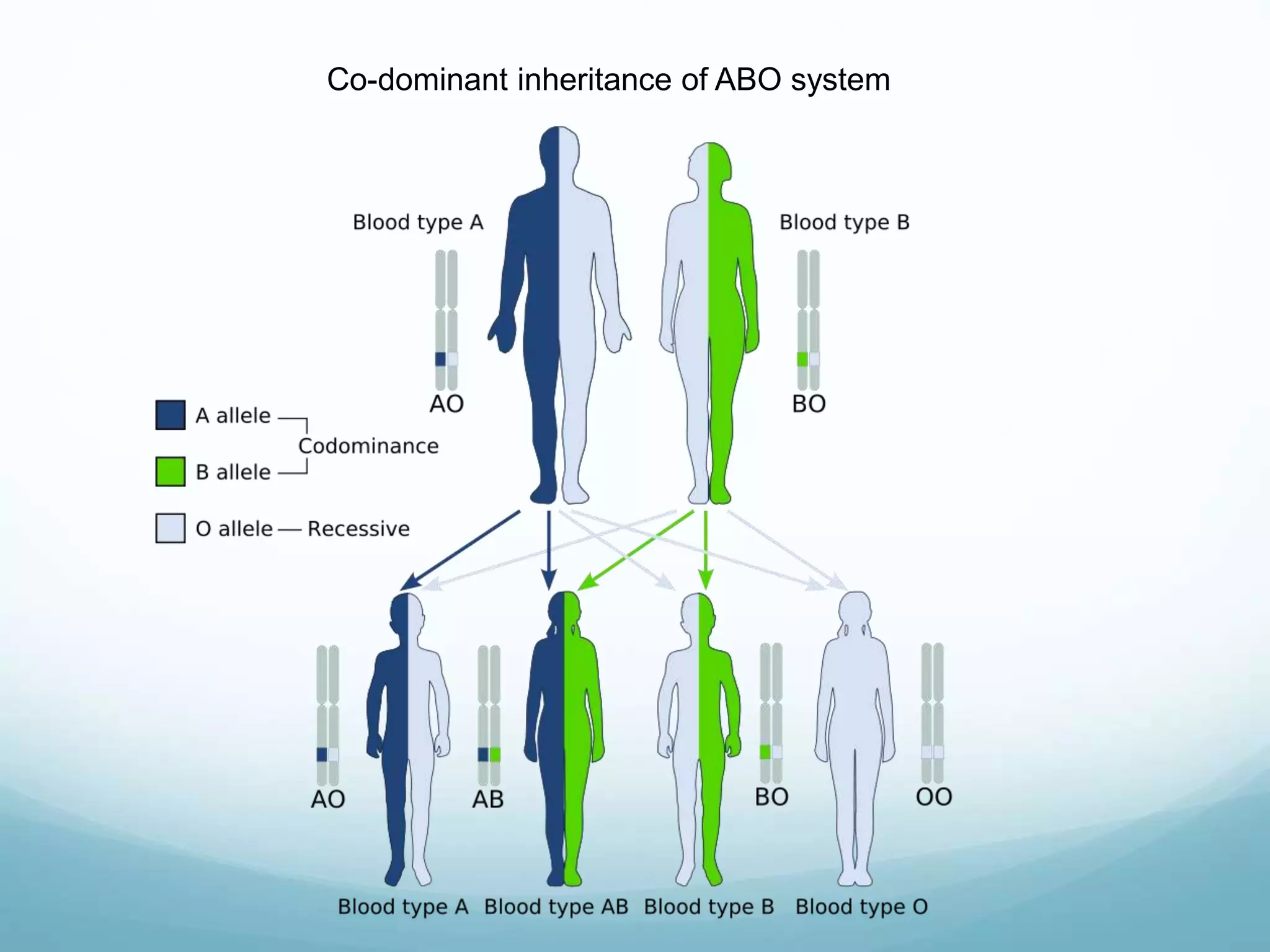
- ABO incompatibility can cause hemolytic disease of the newborn (HDN), occurring in about 25% of pregnancies when the mother's blood type is O and the fetus's is A, B, or AB.
- The disease is caused by IgG antibodies from the mother's blood crossing the placenta and reacting against antigens on the fetus/newborn's red blood cells.
- Diagnosis involves testing the newborn's blood type and bilirubin levels as well as direct Coombs testing of the mother's antibodies.
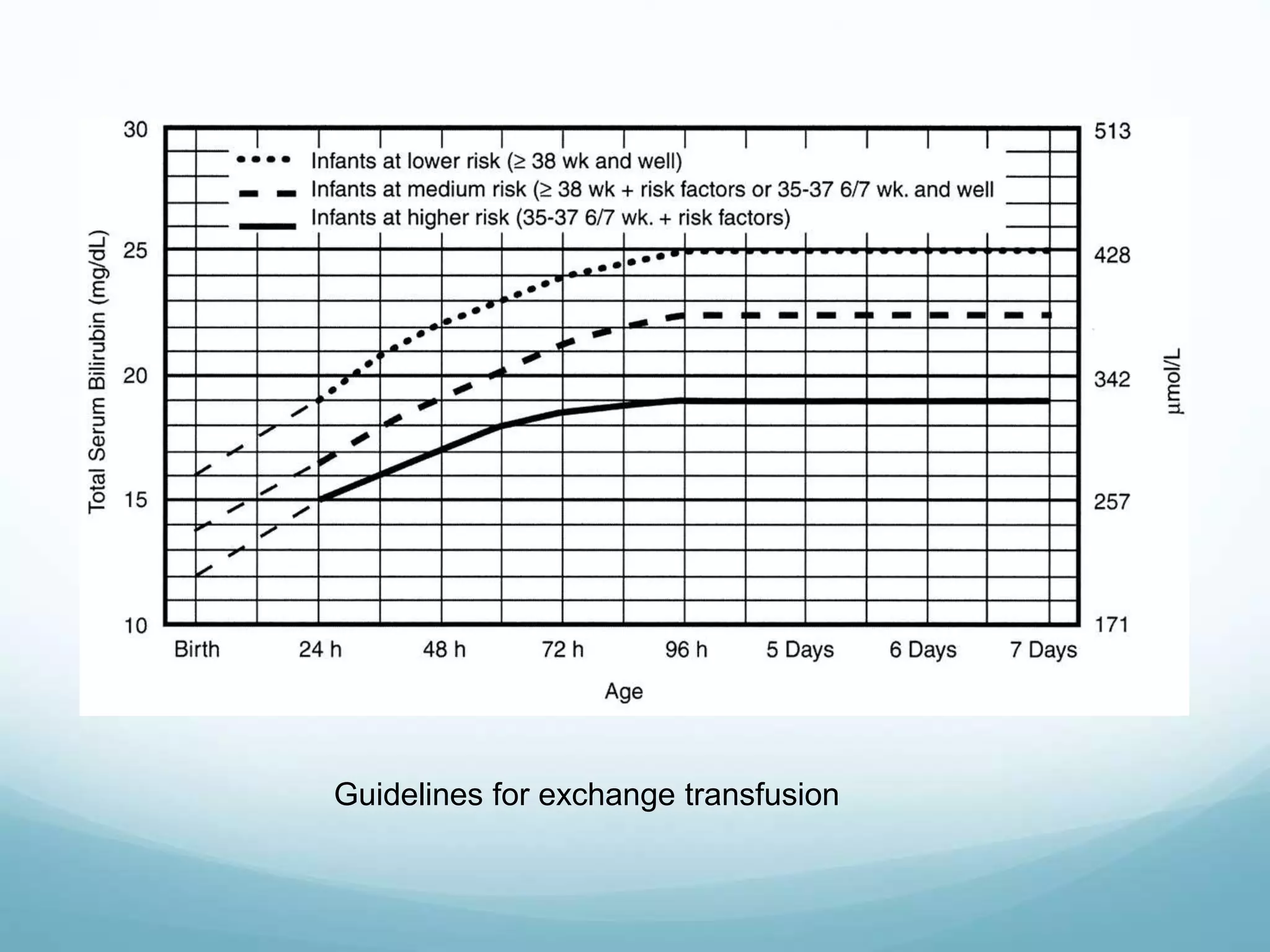
- Management focuses on phototherapy or