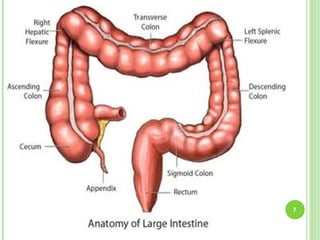
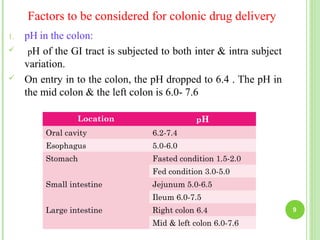
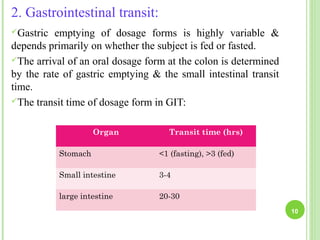
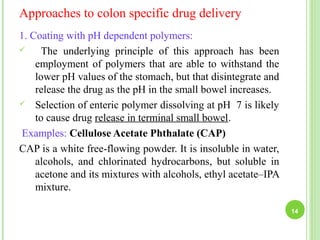
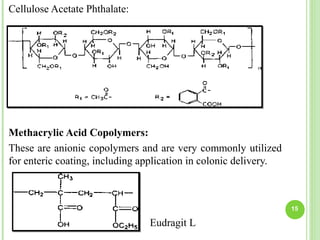
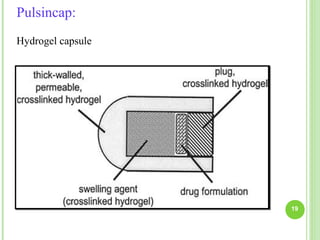
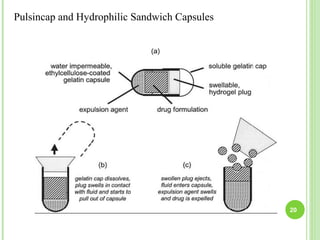
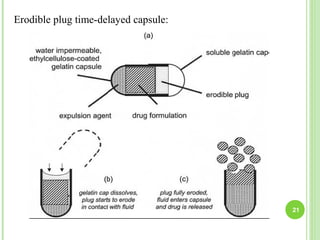
This document provides an overview of colon specific drug delivery systems. It discusses the advantages of targeting drug delivery to the colon which includes reduced dosing, lower side effects, and improved patient compliance. It also reviews some limitations such as multiple manufacturing steps and potential for drug degradation by colonic microflora. The document then examines the anatomy and physiology of the colon, factors that influence colonic drug delivery such as pH and transit time, and how drugs are absorbed in the colon. It concludes by outlining several approaches to colon specific drug delivery including pH dependent coatings, time release systems, prodrugs activated by colonic bacteria, and the use of carriers degraded by colonic microflora.