The document provides information about the male reproductive system, including:
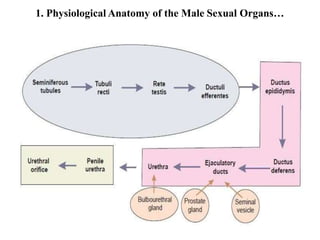
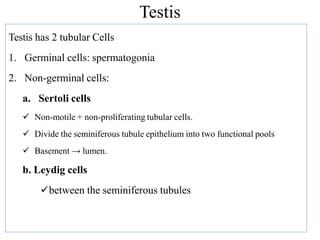
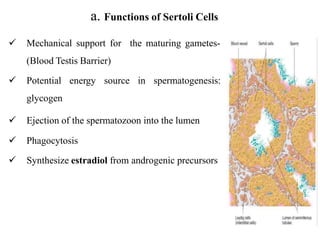
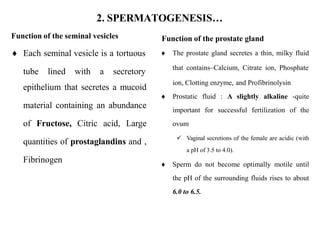
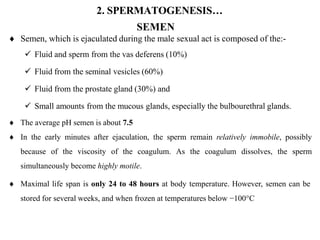
1. It describes the anatomy of the male reproductive organs including the testes, epididymis, vas deferens, seminal vesicles, prostate gland, and urethra.
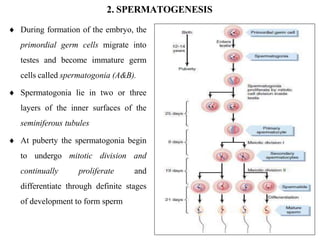
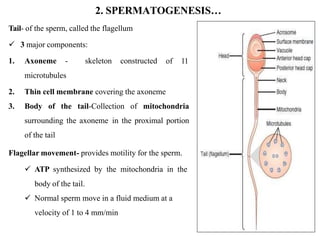
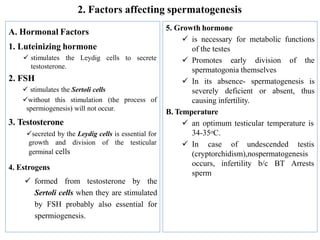
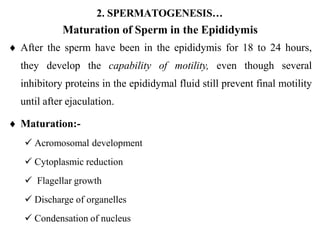
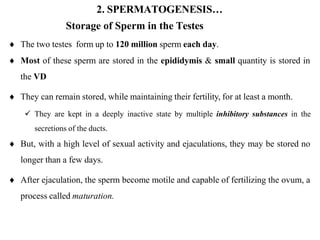
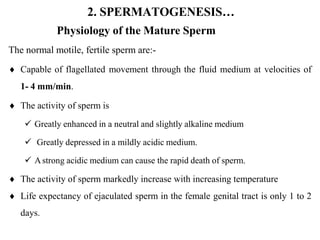
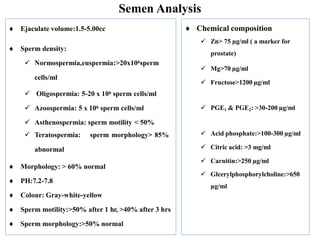
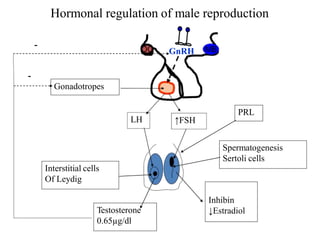
2. It explains spermatogenesis, the process of sperm production and maturation. Key steps include spermatogenesis in the testes and maturation in the epididymis.
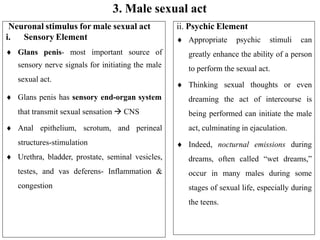
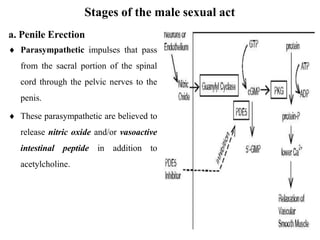
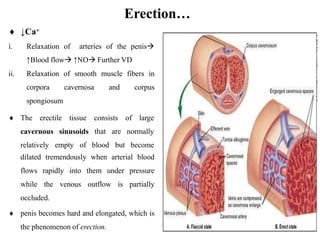
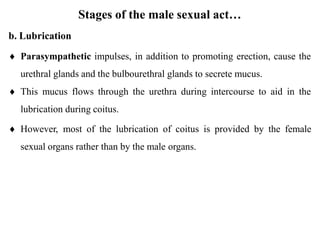
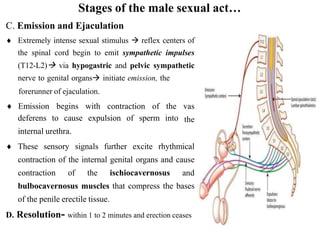
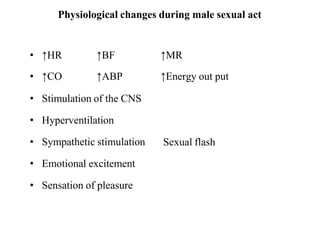
3. It outlines the stages of the male sexual act including penile erection, lubrication, emission of sperm from the vas deferens, and ejaculation through contractions of internal organs and muscles.