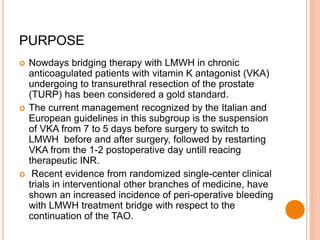
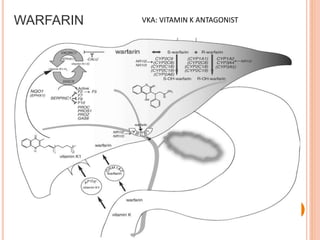
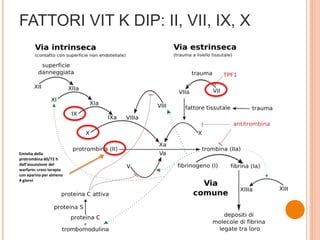
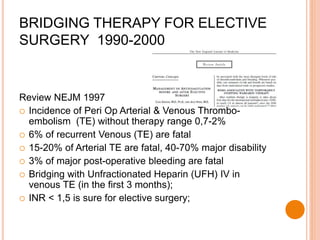
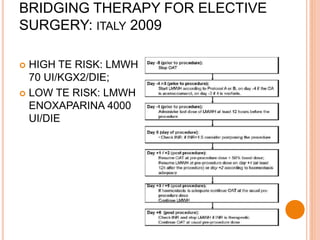
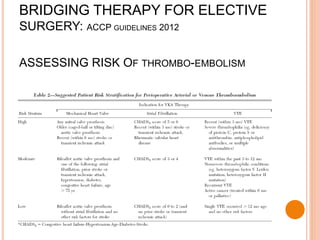
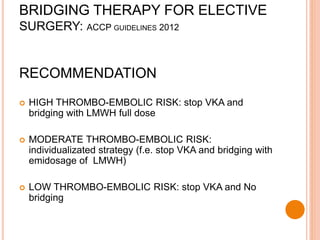
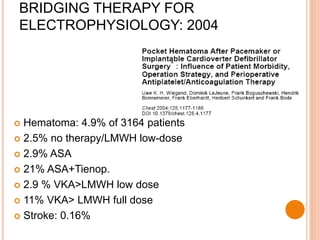
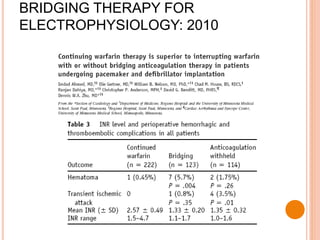
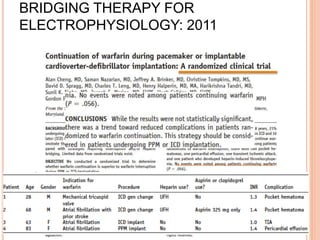
1) The document discusses guidelines for bridging anticoagulation therapy for patients on vitamin K antagonists (VKAs) undergoing elective urological procedures.
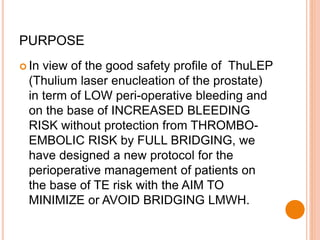
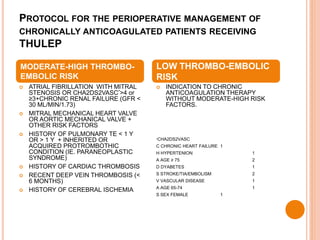
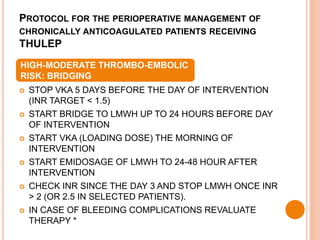
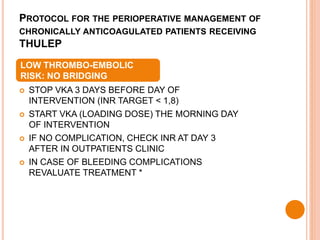
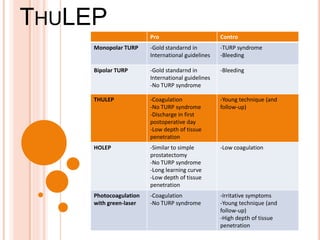
2) It proposes a new protocol for patients undergoing ThuLEP which stratifies thromboembolic risk and minimizes or avoids bridging with low molecular weight heparin (LMWH).
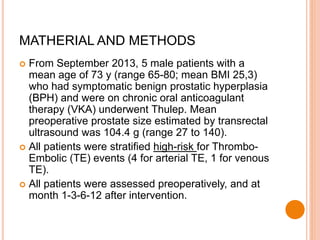
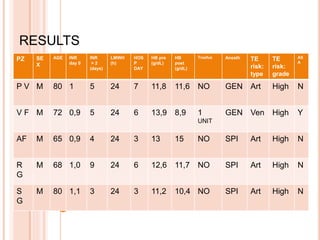
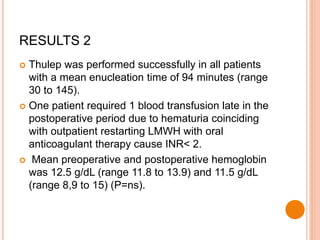
3) Preliminary results from 5 patients managed under the new protocol found it was safe and allowed for shorter hospitalization without thromboembolic or bleeding complications compared to standard bridging therapy.
![BACKGROUND: EXPERIENCE IN UROLOGY
HOLMIUM LASER ENUCLEATION
Holmium laser enucleation of the prostate in
patients on anticoagulant therapy or with
bleeding disorders. Elzayat E J Urol. 2006
Safety of holmium laser enucleation of the
prostate in anticoagulated patients. Tyson MB J
Endourol. 2009
Holmium laser enucleation of the prostate
(HoLEP) in patients with continuous oral
anticoagulation: first reported cases in Japan].
Hirayama T Nihon Hinyokika Gakkai Zasshi. 2010](https://image.slidesharecdn.com/14-150114074925-conversion-gate01/85/Anemo-2014-Infusino-Protocol-anticoagulation-in-urology-23-320.jpg)