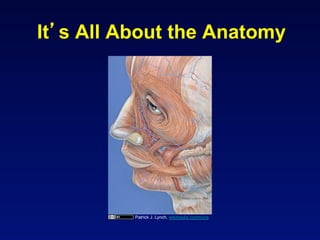
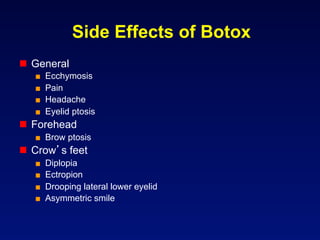
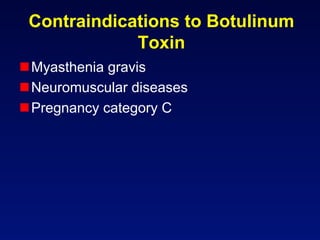
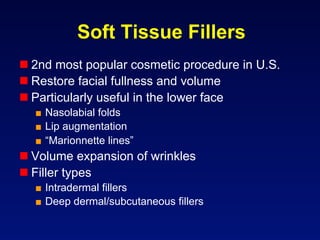
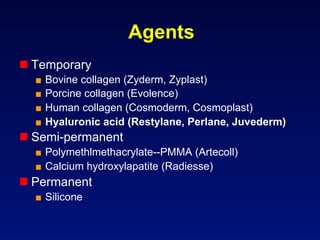
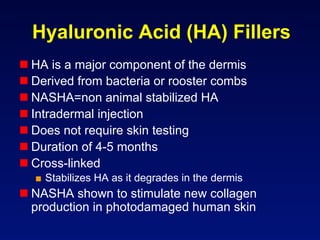
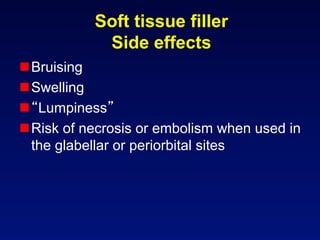
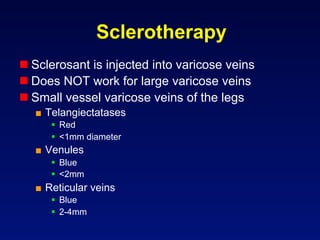
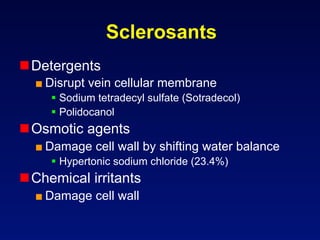
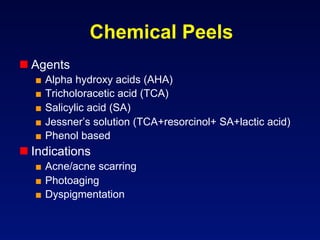
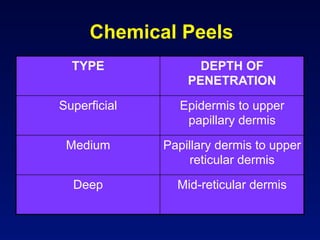
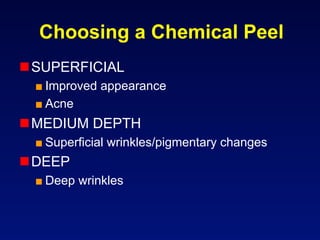
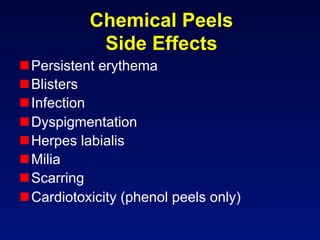
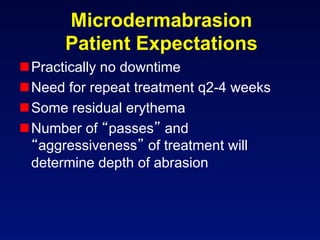
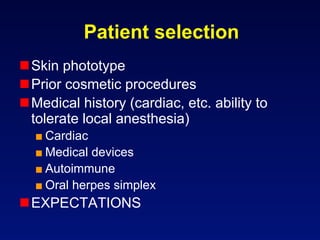
This document discusses various cosmetic dermatology procedures used to improve the appearance of aging skin. It describes how botulinum toxin (Botox) is used to reduce wrinkles by weakening facial muscles. Soft tissue fillers like hyaluronic acid can restore volume to areas like lips and nasolabial folds. Sclerotherapy involves injecting sclerosing agents into spider veins. Chemical peels exfoliate the skin to improve acne scarring, pigmentation issues, and dullness. Microdermabrasion gently abrades the skin's surface. Proper patient selection considers medical history and expectations for these appearance-enhancing treatments.