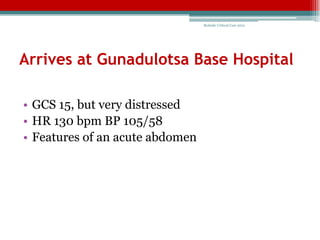
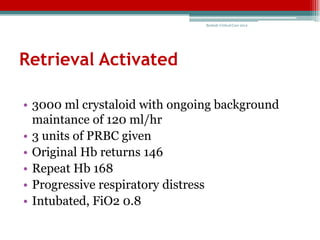
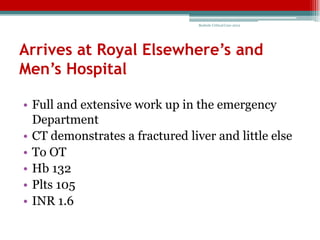
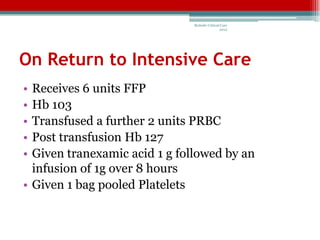
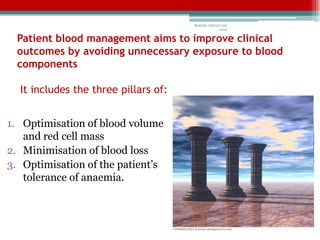
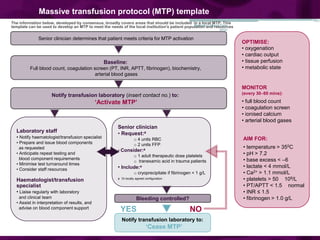
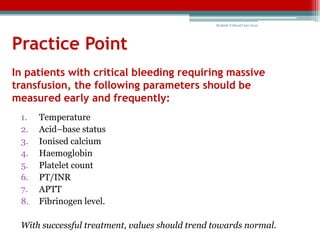
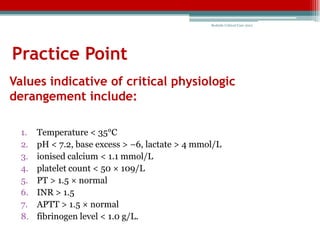
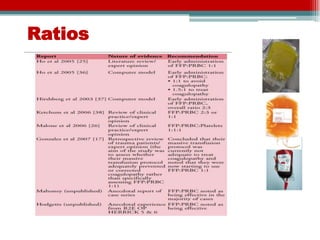
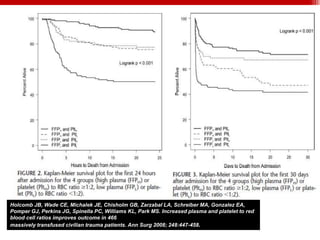
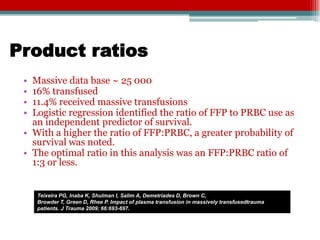
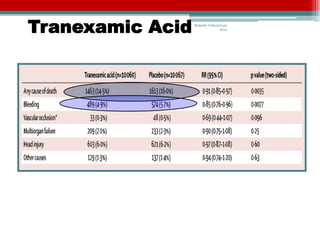
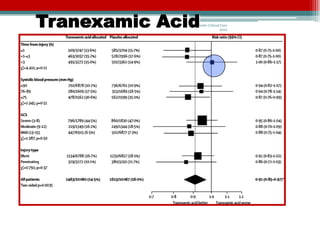
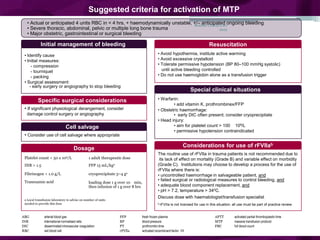
This document discusses transfusion and massive transfusion protocols. It provides a case study of a patient who suffered injuries from a motorcycle accident and received multiple blood transfusions. It then outlines lessons learned, including the importance of massive transfusion protocols, transfusion triggers, transfusion ratios, and the role of tranexamic acid. It recommends hospitals develop massive transfusion protocols and lists critical parameters that should be measured early and frequently for patients receiving massive transfusions, such as temperature, acid-base status, coagulation factors, and hematologic values.