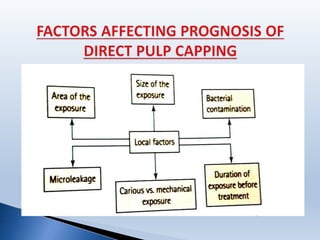
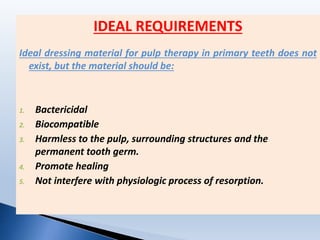
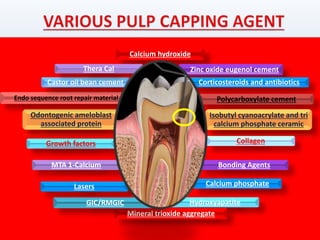
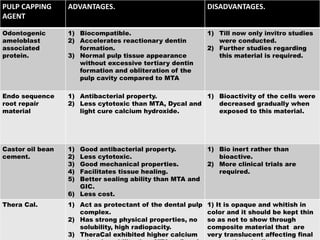
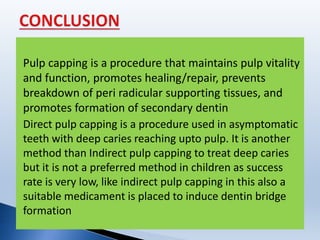
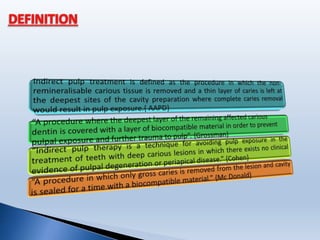
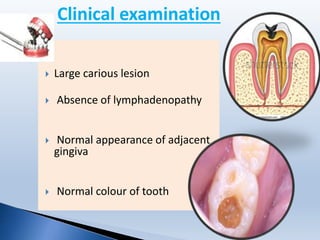
This document summarizes different techniques for pulp capping including direct and indirect pulp capping. It discusses the history of various materials used for pulp capping such as calcium hydroxide and mineral trioxide aggregate. Key points covered include the indications and contraindications for pulp capping, the ideal properties of capping materials, and the histological response after pulp capping including zone formation. The document provides an overview of pulp capping procedures and factors influencing their success.










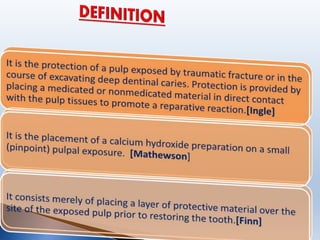
![Placement of a medicated or a nonmedicated material on a pulp that
has been exposed in the course of preparing a cavity in a carious
tooth or as the result of trauma.[Kopel, 1997]
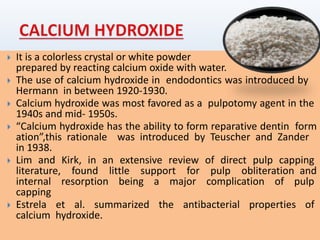
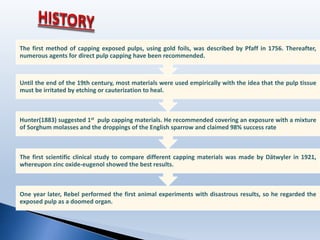
Since then, calcium hydroxide has been recommended by several
authors for direct pulp capping, but it took until the middle of 20th
century until it was regarded as the standard of care.
In 1920 Hermann, introduced calcium hydroxide for root canal fillings.
Between 1928 and 1930 he studied the reaction of vital pulp tissue to
calcium hydroxide to prove that it was a biocompatible material.](https://image.slidesharecdn.com/pulpcappingoroginal-160709063111/85/Pulp-capping-35-320.jpg)

![Localization of infection & inflammation in primary teeth is poorer than
in permanent teeth. [Mc Donalds,1956]
Incidence of reparative dentin formation in primary teeth is more
extensive than permanent Teeth. [Sayegh , 1968]
Primary pulp contain high cellular content which might be responsible
for failures. Primary pulp responds more rapidly to the effects of
dentinal caries then the perm. Teeth. [Rayner & Southam, 1979]
Undifferentiated mesenchymal cells may differentiate into osteoclasts
in response to caries or pulp capping material which could lead to
internal resorption. [Kennedy,1985]](https://image.slidesharecdn.com/pulpcappingoroginal-160709063111/85/Pulp-capping-40-320.jpg)
![Primary Pulp are more closer to outer enamel surface & are rapidly
infected by the carious lesion. Once exposed pulpal inflammation is so
involved that the DPC proves unfavorable. [Kennedy & Kopel,1985]
Increased resorption in primary teeth is because already root resorption
is in progress. [Stanley, 1985]
Wide apical foramina in pri. teeth leads to abundant blood supply which
results in more typical and faster inflammation response to irritation than
in permanent teeth. [Kopel,1992]
Acc. To finn, in primary teeth pulp capping is best carried out in teeth
where dental pulp has been mechanically exposed.
Pulp capping not recommended. Internal resorption or acute
dentoalveolar abscess may result . [Pinkham]](https://image.slidesharecdn.com/pulpcappingoroginal-160709063111/85/Pulp-capping-41-320.jpg)