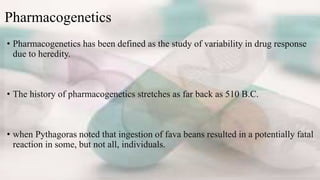
Pharmacogenetics is the study of how genetics affect individual responses to drugs. Variations in genes like CYP2D6, G6PD, and TPMT can determine drug metabolism and toxicity. Knowing a patient's genetic profile allows doctors to determine the right drug, dosage, and treatment schedule to maximize effectiveness and minimize adverse reactions. For a boy with leukemia, testing revealed a genetic variation that impacts thiopurine metabolism. His doctors were able to adjust his chemotherapy accordingly, preventing toxic side effects and allowing continued treatment. Pharmacogenetics aims to personalize drug therapy based on a patient's unique genetic makeup.
![Example of different response to drugs
• Primaquine-induced hemolytic anemia among African-Americans
• Later shown to be due to glucose-6-phosphate dehydrogenase [G6PD] variant
alleles.
• succinylcholine-induced prolonged apnea during anesthesia (due to autosomal
recessive butyrylcholinesterase deficiency).
• Severe adverse effects after antituberculosis treatment with isoniazid (later
shown to be due to N-acetyltransferase [NAT] variant allele).](https://image.slidesharecdn.com/presentation1-161030084619/85/Presentation1-5-320.jpg)