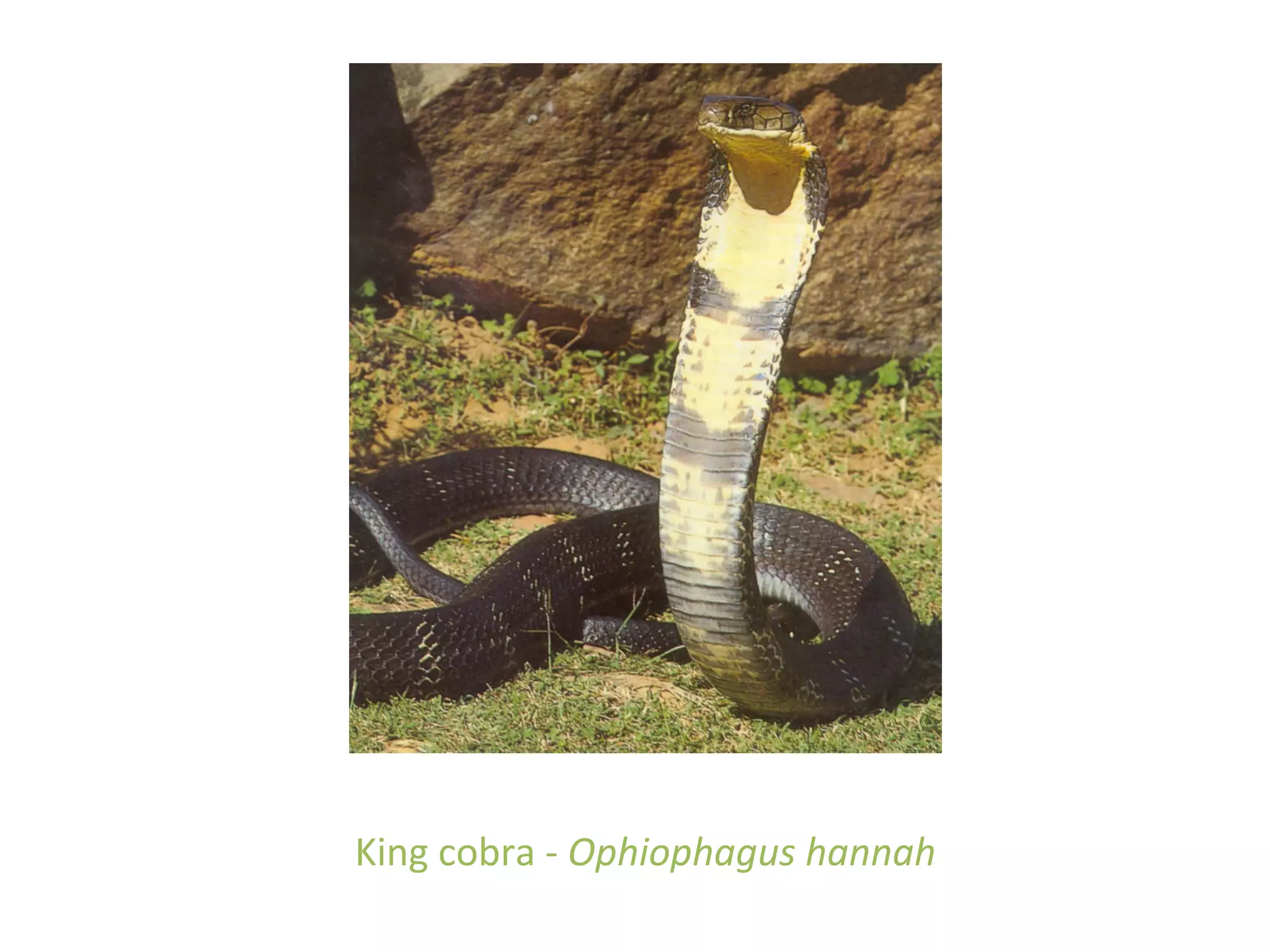
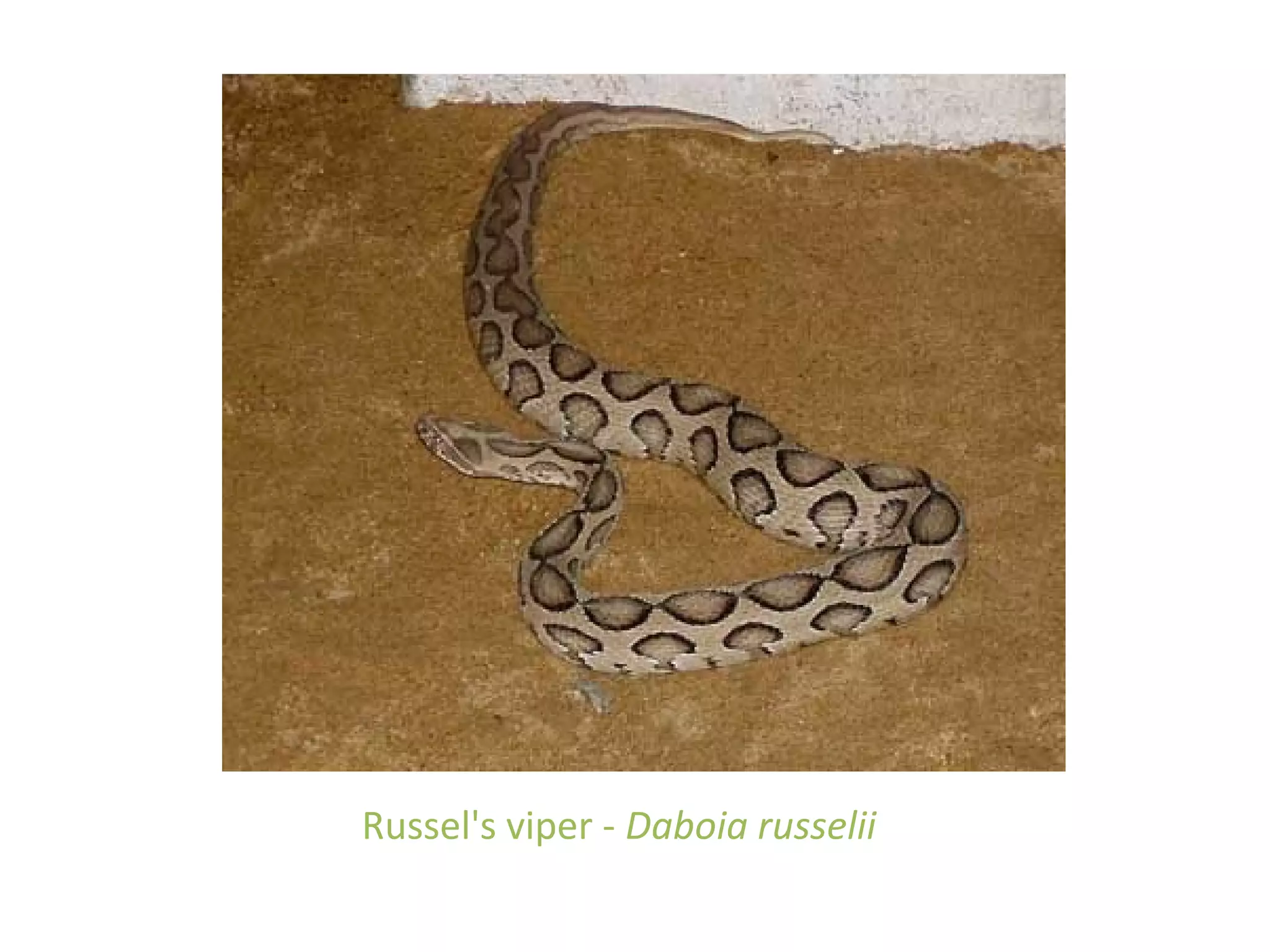
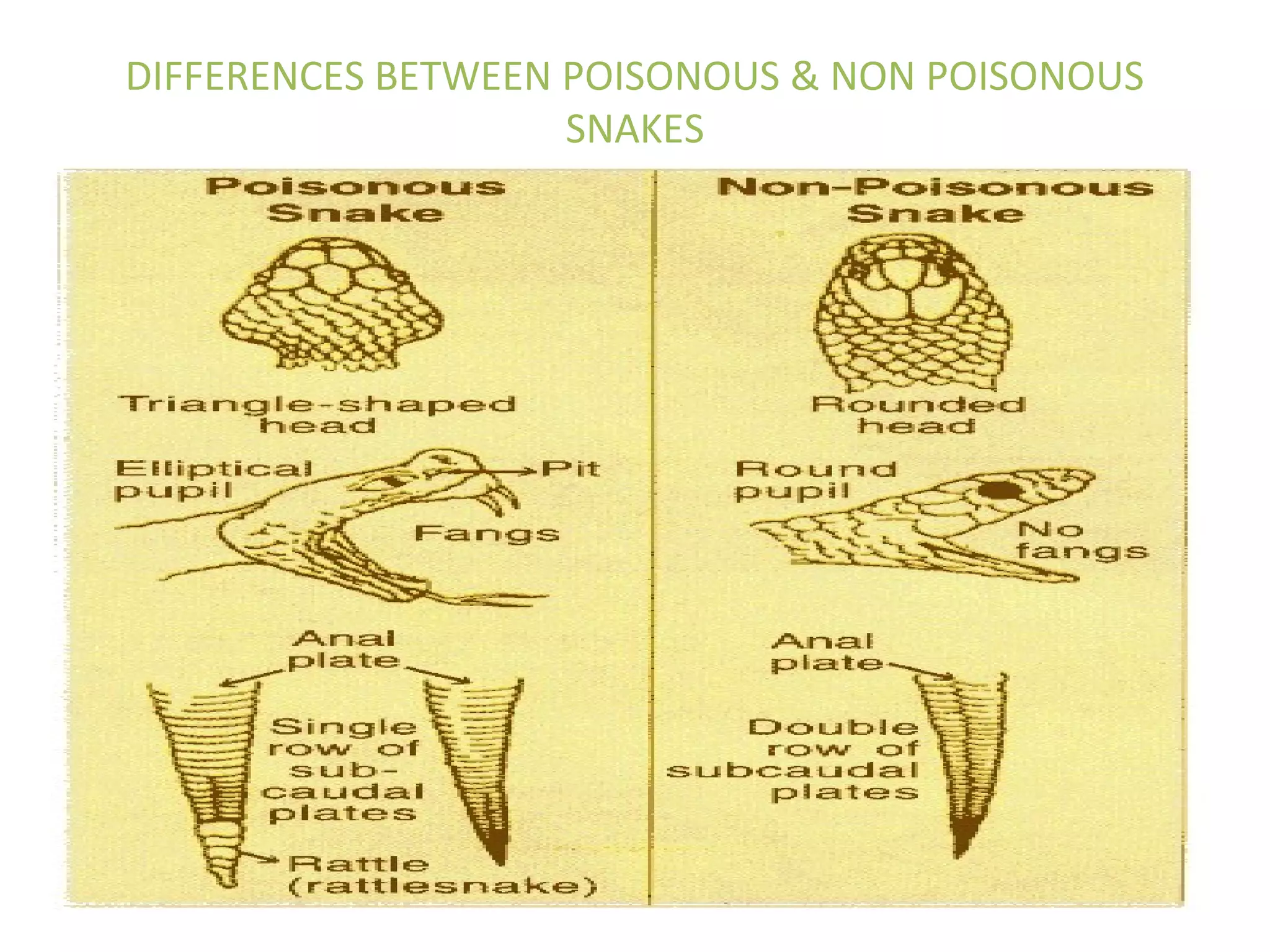
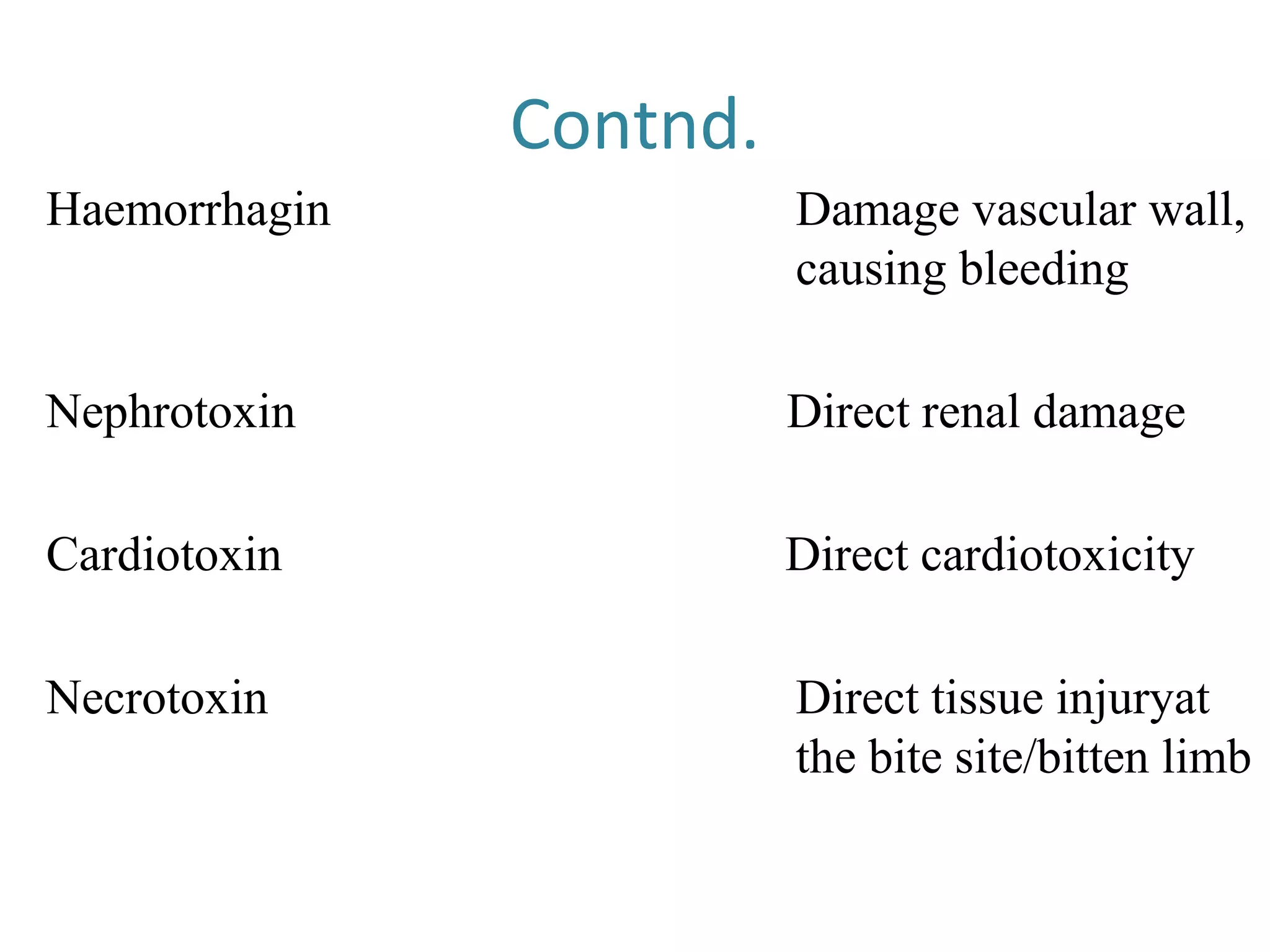
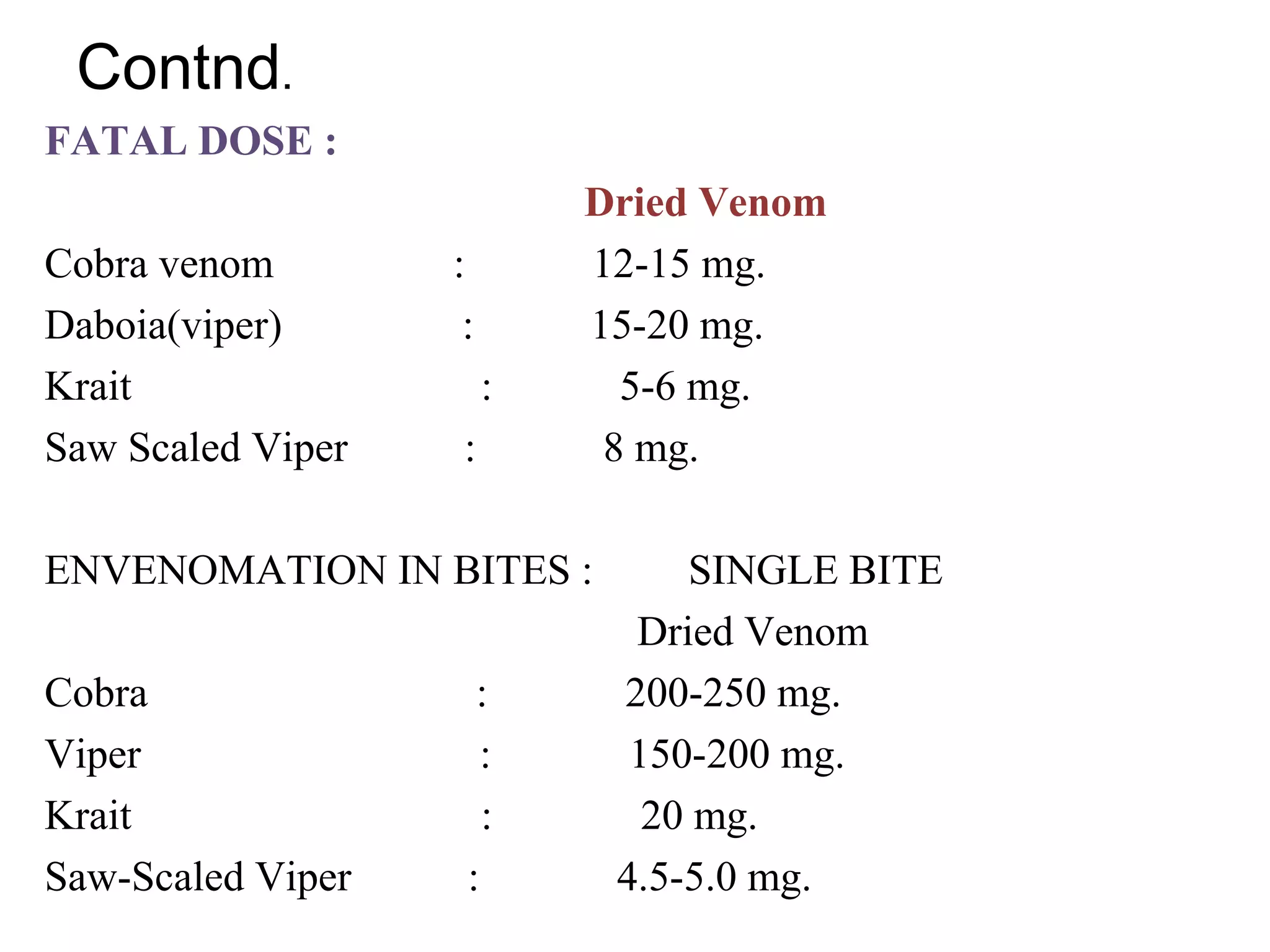
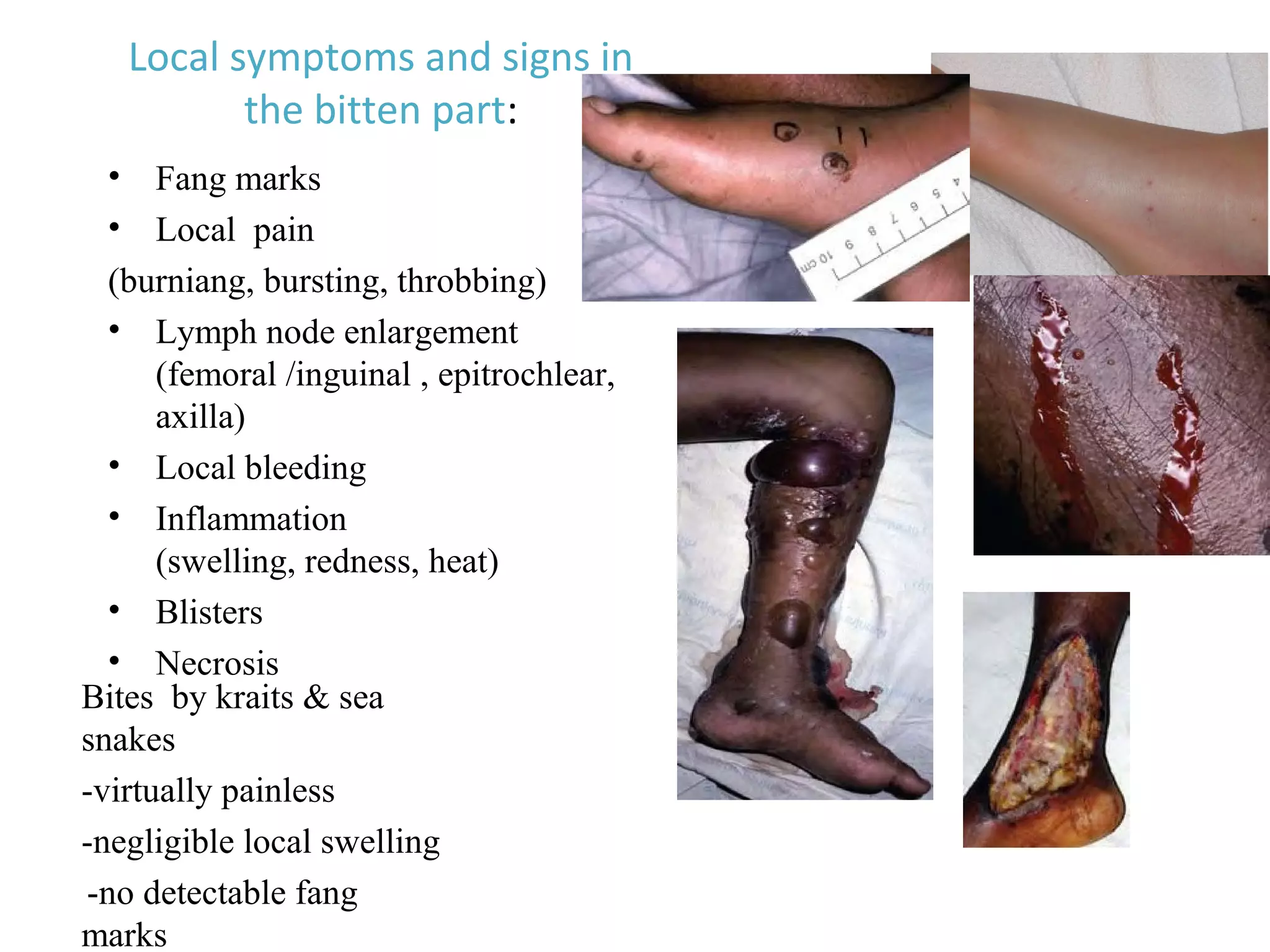
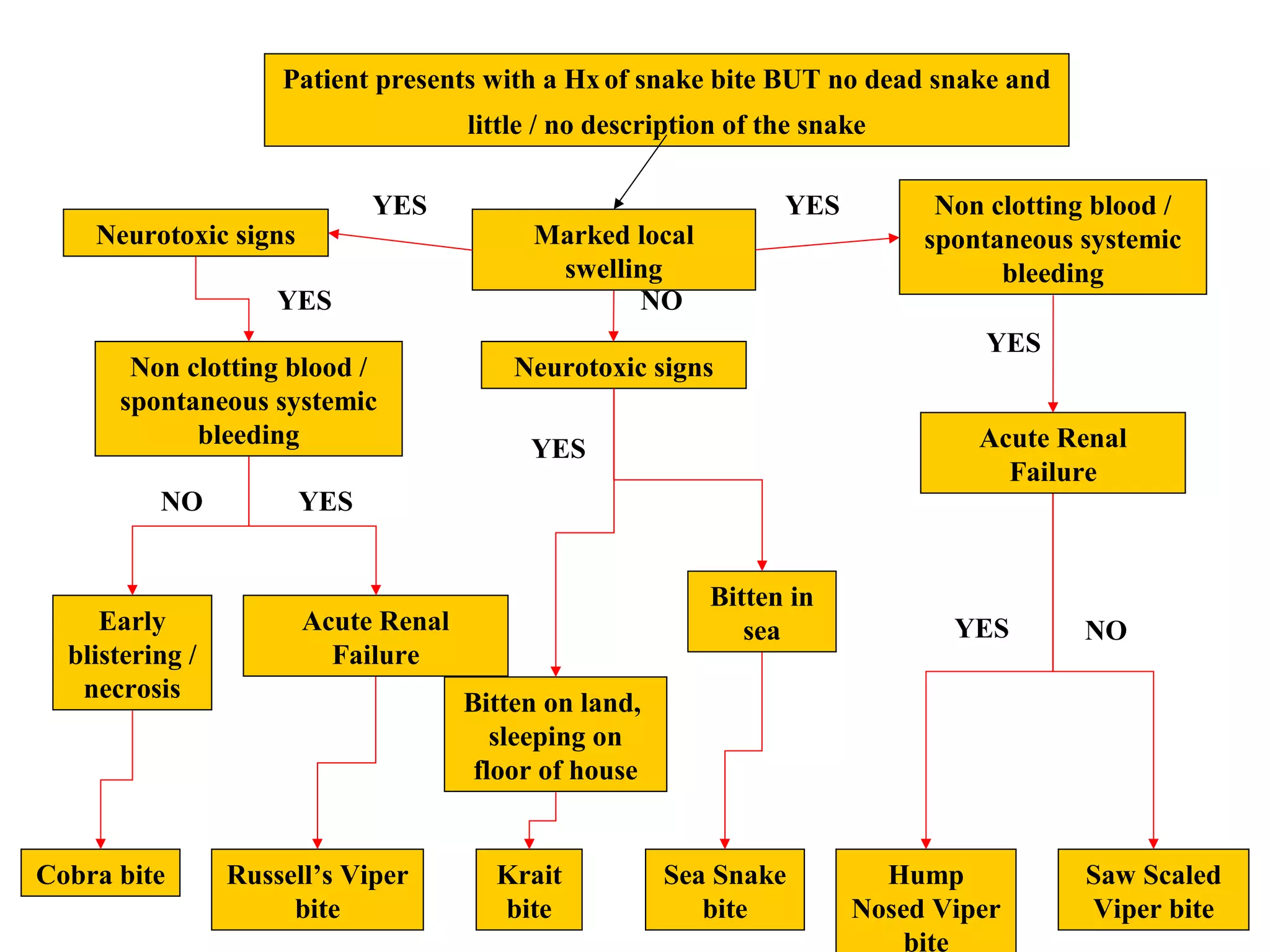
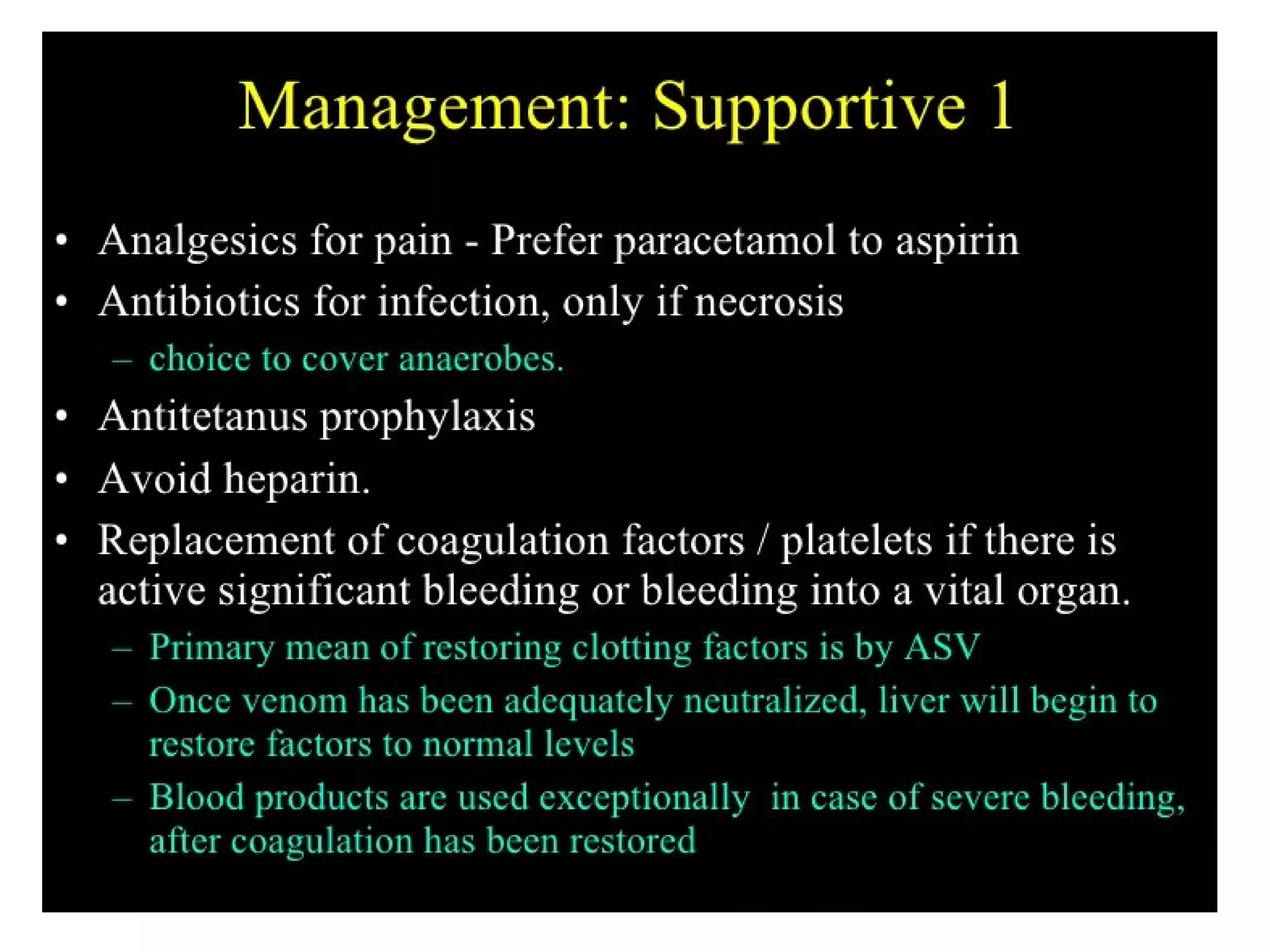
This document discusses snake venom poisoning and its management. It begins by classifying snakes and identifying the 5 families that contain venomous species. It then describes the differences between poisonous and non-poisonous snakes. The document outlines the components of snake venom and their effects. Signs and symptoms of envenomation are provided for different snake families. Diagnosis involves identifying the snake species based on symptoms, circumstances, or antigen detection. Treatment primarily involves administering antivenom, with dosages varying based on severity of symptoms. Adjuvant treatments like neostigmine may also be used depending on the neurotoxin involved.