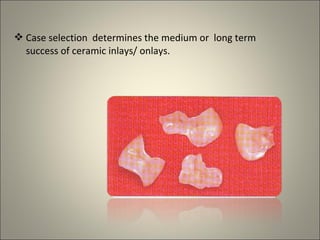
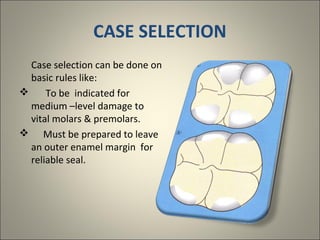
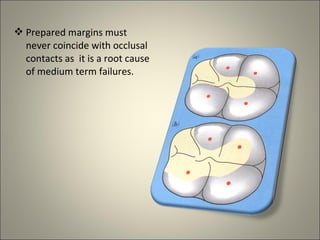
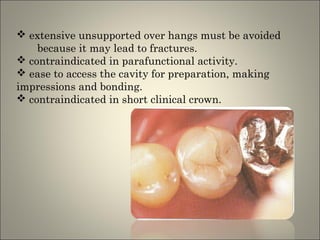
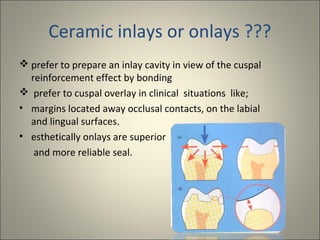
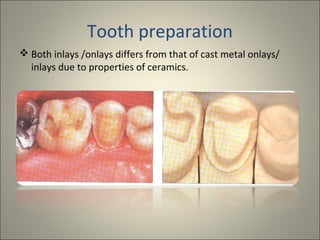
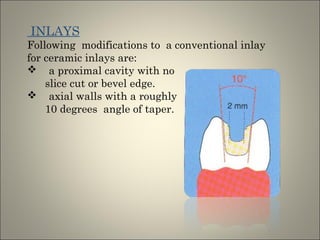
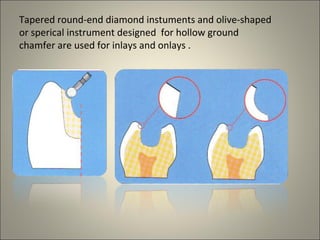
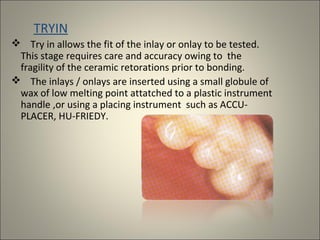
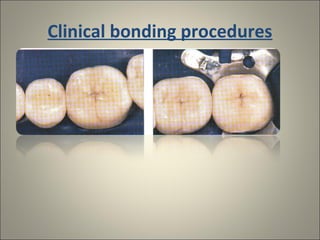
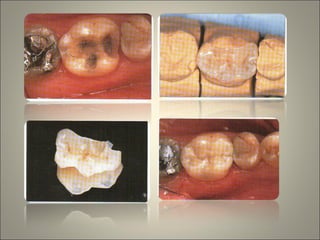
This document discusses ceramic inlays and onlays. It begins by providing a brief history of ceramic inlays and improvements in technology that allowed for their reintroduction in the 1980s. It then discusses case selection criteria, tooth preparation details, fabrication process including impressions, temporization, try-in and adjustments. The document concludes with details on cementation and clinical bonding procedures. Key points covered include contraindications, margin design, choice of cement, importance of adhesion and sealing margins to ensure success.